J Gynecol Oncol.
2013 Jan;24(1):14-20. 10.3802/jgo.2013.24.1.14.
Risk factor analysis of coexisting endometrial carcinoma in patients with endometrial hyperplasia: a retrospective observational study of Taiwanese Gynecologic Oncology Group
- Affiliations
-
- 1Gynecologic Cancer Center, Department of Obstetrics and Gynecology, Cathay General Hospital and Department of Obstetrics and Gynecology, National Taiwan University Hospital, National Taiwan University College of Medicine, Taipei, Taiwan.
- 2Department of Obstetrics and Gynecology, Mackay Memorial Hospital, Mackay Medical College, Department of Nursing, Mackay Medicine, Nursing and Management College, and Department of Obstetrics and Gynecology, Taipei Medical University, Taipei, Taiwan.
- 3Department of Obstetrics and Gynecology, Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Taoyuan, Taiwan.
- 4Department of Obstetrics and Gynecology, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan.
- 5Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Kaohsiung, Taiwan.
- 6Department of Obstetrics and Gynecology, Taichung Veterans General Hospital, Taichung, Taiwan.
- 7Department of Obstetrics and Gynecology, Taipei Veterans General Hospital and Department of Obstetrics and Gynecology, National Yang-Ming University School of Medicine, Taipei, Taiwan. msyen@vghtpe.gov.tw
- 8Department of Obstetrics and Gynecology, China Medical University Hospital, China Medical University College of Medicine, Taichung, Taiwan.
- 9Department of Obstetrics and Gynecology, National Cheng Kung University Hospital, National Cheng Kung University College of Medicine, Tainan, Taiwan.
- KMID: 2288556
- DOI: http://doi.org/10.3802/jgo.2013.24.1.14
Abstract
OBJECTIVE
To evaluate the clinical outcome and parameters related to coexisting endometrial carcinoma in women with tissue-diagnosed endometrial hyperplasia.
METHODS
Between January 1991 and December 2009, three hundred and eighty-six patients with the presumptive diagnosis of endometrial hyperplasia were retrieved. Among these, one hundred and twenty-five patients were identified as having coexisting endometrial carcinoma in hysterectomy specimens. The three hundred and eighty-six patients were divided into two groups: the hyperplasia-benign group (261 cases) and the hyperplasia-malignant group (125 cases). Several clinical parameters including age, menopausal status, history of abnormal uterine bleeding, obstetrical history, medical history of diabetes and hypertension, BMI, and preoperative pathologic results were investigated.
RESULTS
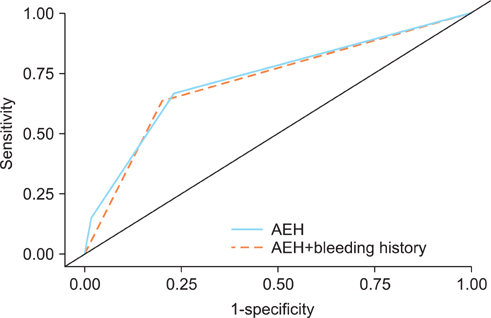
Age > or =53 (odds ratio [OR], 2.40; 95% confidence interval [CI], 1.26 to 4.57), menopausal status (OR, 2.07; 95% CI, 1.14 to 3.76), diabetes history (OR, 7.33; 95% CI, 2.79 to 19.26), abnormal uterine bleeding (OR, 3.99; 95% CI, 1.22 to 13.02), atypical endometrial hyperplasia (OR, 7.38; 95% CI, 4.03 to 13.49), and body mass index > or =27 (OR, 3.24; 95% CI, 1.76 to 5.97) were independent risk factors for prediction of endometrial hyperplasia coexisting with endometrial carcinoma. The diagnostic efficacy of atypical endometrial hyperplasia to predict the endometrial hyperplasia coexisting with endometrial carcinoma was better than or similar to those of other independent factors and combinations of these factors.
CONCLUSION
Coexisting malignancy should be considered when examining endometrial hyperplasia patients with the related risk factors, especially atypical endometrial hyperplasia.
MeSH Terms
Figure
Cited by 1 articles
-
Non-atypical endometrial hyperplasia: risk factors for occult endometrial atypia and malignancy in patients managed with hysterectomy
Lee Shi Hui, Selina Hui Men Chin, Charissa Goh, Lin Xiao Hui, Manisha Mathur, Timothy Lim Yong Kuei, Felicia Chin Hui Xian
Obstet Gynecol Sci. 2021;64(3):300-308. doi: 10.5468/ogs.20294.
Reference
-
1. Trimble CL, Kauderer J, Zaino R, Silverberg S, Lim PC, Burke JJ 2nd, et al. Concurrent endometrial carcinoma in women with a biopsy diagnosis of atypical endometrial hyperplasia: a Gynecologic Oncology Group study. Cancer. 2006. 106:812–819.2. Kurman RJ, Kaminski PF, Norris HJ. The behavior of endometrial hyperplasia: a long-term study of "untreated" hyperplasia in 170 patients. Cancer. 1985. 56:403–412.3. Montgomery BE, Daum GS, Dunton CJ. Endometrial hyperplasia: a review. Obstet Gynecol Surv. 2004. 59:368–378.4. Baak JP, Mutter GL, Robboy S, van Diest PJ, Uyterlinde AM, Orbo A, et al. The molecular genetics and morphometry-based endometrial intraepithelial neoplasia classification system predicts disease progression in endometrial hyperplasia more accurately than the 1994 World Health Organization classification system. Cancer. 2005. 103:2304–2312.5. Mutter GL. The Endometrial Collaborative Group. Endometrial intraepithelial neoplasia (EIN): will it bring order to chaos? Gynecol Oncol. 2000. 76:287–290.6. Shutter J, Wright TC Jr. Prevalence of underlying adenocarcinoma in women with atypical endometrial hyperplasia. Int J Gynecol Pathol. 2005. 24:313–318.7. Chen YL, Cheng WF, Lin MC, Huang CY, Hsieh CY, Chen CA. Concurrent endometrial carcinoma in patients with a curettage diagnosis of endometrial hyperplasia. J Formos Med Assoc. 2009. 108:502–507.8. Announcements: FIGO stages 1988 revision. Gynecol Oncol. 1989. 35:125–126.9. Soslow RA. Problems with the current diagnostic approach to complex atypical endometrial hyperplasia. Cancer. 2006. 106:729–731.10. Merisio C, Berretta R, De Ioris A, Pultrone DC, Rolla M, Giordano G, et al. Endometrial cancer in patients with preoperative diagnosis of atypical endometrial hyperplasia. Eur J Obstet Gynecol Reprod Biol. 2005. 122:107–111.11. Dunton CJ, Baak JP, Palazzo JP, van Diest PJ, McHugh M, Widra EA. Use of computerized morphometric analyses of endometrial hyperplasias in the prediction of coexistent cancer. Am J Obstet Gynecol. 1996. 174:1518–1521.12. Kurman RJ, Norris HJ. Evaluation of criteria for distinguishing atypical endometrial hyperplasia from well-differentiated carcinoma. Cancer. 1982. 49:2547–2559.13. Widra EA, Dunton CJ, McHugh M, Palazzo JP. Endometrial hyperplasia and the risk of carcinoma. Int J Gynecol Cancer. 1995. 5:233–235.14. Mylonas I, Makovitzky J, Richter DU, Jeschke U, Briese V, Friese K. Expression of the inhibin-alpha subunit in normal, hyperplastic and malignant endometrial tissue: an immunohistochemical analysis. Gynecol Oncol. 2004. 93:92–97.15. Matias-Guiu X, Catasus L, Bussaglia E, Lagarda H, Garcia A, Pons C, et al. Molecular pathology of endometrial hyperplasia and carcinoma. Hum Pathol. 2001. 32:569–577.16. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003. 348:1625–1638.17. Sjostrom L, Narbro K, Sjostrom CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007. 357:741–752.18. Fader AN, Arriba LN, Frasure HE, von Gruenigen VE. Endometrial cancer and obesity: epidemiology, biomarkers, prevention and survivorship. Gynecol Oncol. 2009. 114:121–127.19. Tao MH, Freudenheim JL. DNA methylation in endometrial cancer. Epigenetics. 2010. 5:491–498.20. Cohn DE, Fabbri M, Valeri N, Alder H, Ivanov I, Liu CG, et al. Comprehensive miRNA profiling of surgically staged endometrial cancer. Am J Obstet Gynecol. 2010. 202:656.e1–656.e8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coexisting carcinoma in endometrial hyperplasia: does more risk factor mean better discrimination?
- Response to comment on: Comparison of diagnostic accuracy between endometrial curettage and aspiration biopsy in patients treated with progestin for endometrial hyperplasia: a Korean Gynecologic Oncology Group study
- Letter to editor in response to: Comparison of diagnostic accuracy between endometrial curettage and aspiration biopsy in patients treated with progestin for endometrial hyperplasia: a Korean Gynecologic Oncology Group study
- Present status and future direction of clinical trials in advanced endometrial carcinoma
- The clinical approach for endometrial biopsies with atypical endometrial hyperplasia for further management