J Breast Cancer.
2012 Dec;15(4):462-467. 10.4048/jbc.2012.15.4.462.
Simultaneous Chest Wall Reconstruction after Sternectomy and Modified Radical Mastectomy in Locally Advanced Breast Cancer with Solitary Sternal Metastasis
- Affiliations
-
- 1Department of Surgery, Konkuk University Chungju Hospital, Konkuk University School of Medicine, Chungju, Korea.
- 2Department of Thoracic and Cardiovascular Surgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 3Department of Surgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. 0117652771@kuh.ac.kr
- KMID: 2286445
- DOI: http://doi.org/10.4048/jbc.2012.15.4.462
Abstract
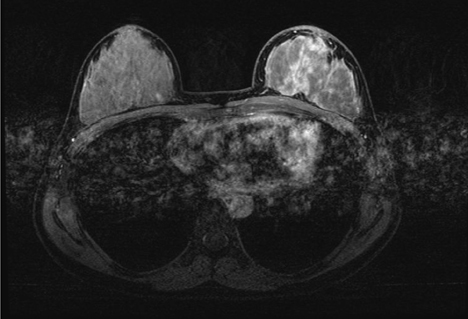
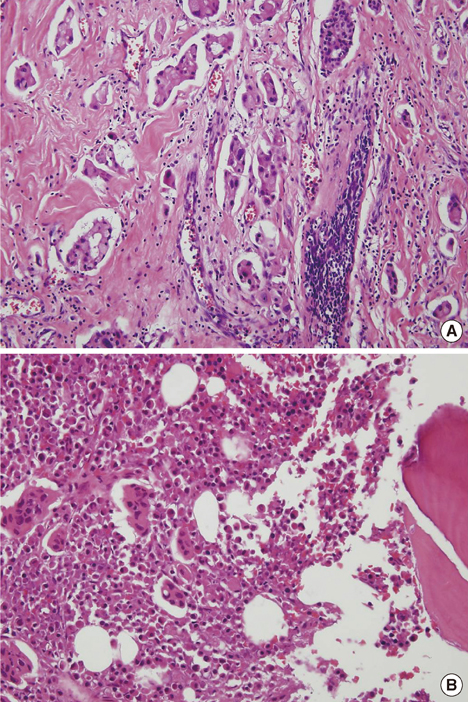
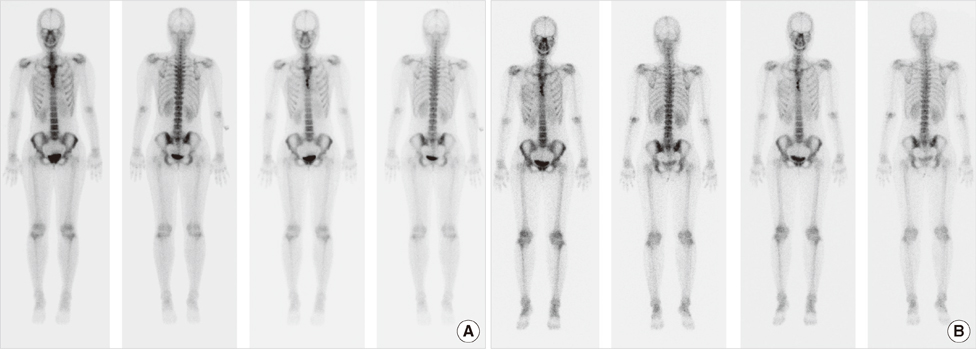
- Bone is the most common metastatic organ in patients with breast cancer. The most significant clinical symptom of bone metastasis is pain which reduces quality of life in cancer patients. We report a case of chest wall reconstruction after partial sternal resection for solitary sternal metastasis and modified radical mastectomy in a patient with locally advanced breast cancer. The sternal defect was reconstructed with a 2 mm thick Gore-Tex patch. Postoperative pain was acceptable and the patient was discharged without any complications. The patient received the endocrine and bisphosphonate therapy combined with chemotherapy and radiotherapy. No recurrence or complications were observed during a follow-up period of 36 months. We describe our good surgical management results of sternal metastatic lesion in a patient with locally advanced breast cancer. We suggest that simultaneous sternectomy is a safe and curative surgical method for a solitary sternal metastasis when no evidence of systemic spread is noted.
Keyword
MeSH Terms
Figure
Reference
-
1. Kwai AH, Stomper PC, Kaplan WD. Clinical significance of isolated scintigraphic sternal lesions in patients with breast cancer. J Nucl Med. 1988. 29:324–328.2. Noguchi S, Miyauchi K, Nishizawa Y, Imaoka S, Koyama H, Iwanaga T. Results of surgical treatment for sternal metastasis of breast cancer. Cancer. 1988. 62:1397–1401.
Article3. Brower ST, Weinberg H, Tartter PI, Camunas J. Chest wall resection for locally recurrent breast cancer: indications, technique, and results. J Surg Oncol. 1992. 49:189–195.
Article4. Park HM, Tarver RD. Solitary sternal metastasis from breast carcinoma. Clin Nucl Med. 1983. 8:373–374.
Article5. Veronesi G, Scanagatta P, Goldhirsch A, Rietjens M, Colleoni M, Pelosi G, et al. Results of chest wall resection for recurrent or locally advanced breast malignancies. Breast. 2007. 16:297–302.
Article6. Lequaglie C, Massone PP, Giudice G, Conti B. Analysis and long-term survival in sternectomy with plastic reconstruction for primary and secondary neoplasms of the sternum. Chir Ital. 2001. 53:485–494.7. Lequaglie C, Massone PB, Giudice G, Conti B. Gold standard for sternectomies and plastic reconstructions after resections for primary or secondary sternal neoplasms. Ann Surg Oncol. 2002. 9:472–479.
Article8. Arnold PG, Pairolero PC. Chest-wall reconstruction: an account of 500 consecutive patients. Plast Reconstr Surg. 1996. 98:804–810.
Article9. Halm HF, Hoffmann C, Winkelmann W. The use of a Gore-Tex soft-tissue patch to repair large full-thickness defects after subtotal sternectomy. A report of three cases. J Bone Joint Surg Am. 2001. 83A:420–423.10. Wuisman P, Scheld H, Tjan T, Roessner A, Blasius S, Vestring T, et al. Chondromyxoid fibroma of the sternum. Case report. Arch Orthop Trauma Surg. 1993. 112:255–256.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Immediate Breast and Chest Wall Reconstruction for Advanced Breast Cancer
- External Oblique Myocutaneous Flap for Reconstruction of Large Chest-Wall Defects following Resection of Advanced Breast Cancer
- Sternal defect reconstruction using a double-barrel vascularized free fibula flap: a case report
- Simultaneous forequarter amputation and radical mastectomy for metastatic breast carcinoma in a male patient: a case report
- Sternal Resection and Reconstruction for Solitary Plasmacytoma of the Sternum: Case Report