J Breast Cancer.
2013 Jun;16(2):236-243. 10.4048/jbc.2013.16.2.236.
Abdominal Advancement Flap as Oncoplastic Breast Conservation: Report of Seven Cases and Their Cosmetic Results
- Affiliations
-
- 1Department of Breast Surgery, Mie University Graduate School of Medicine, Tsu, Japan. mokomoko@clin.medic.mie-u.ac.jp
- KMID: 2286407
- DOI: http://doi.org/10.4048/jbc.2013.16.2.236
Abstract
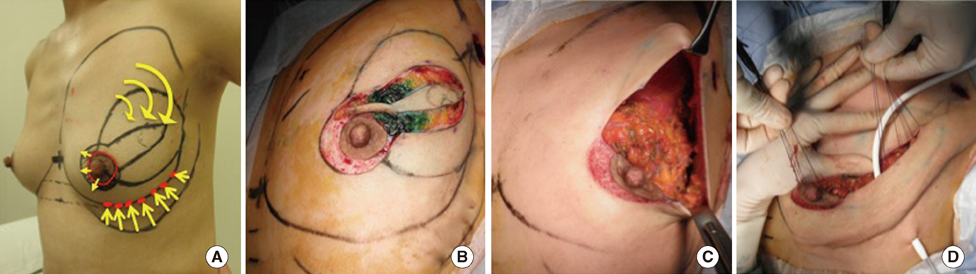
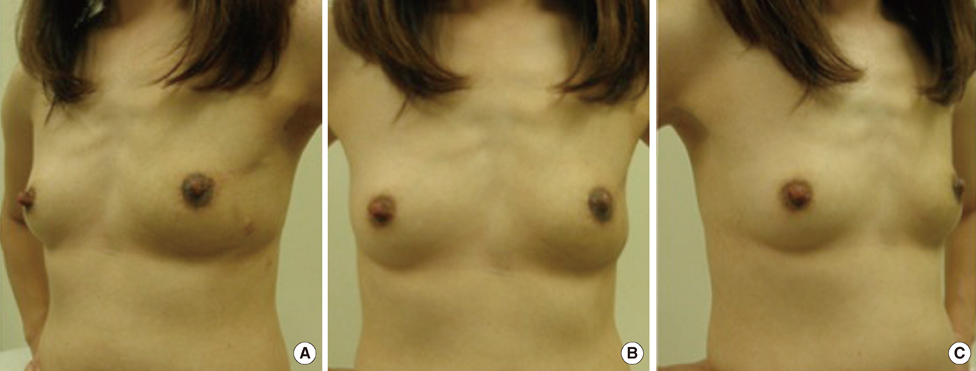
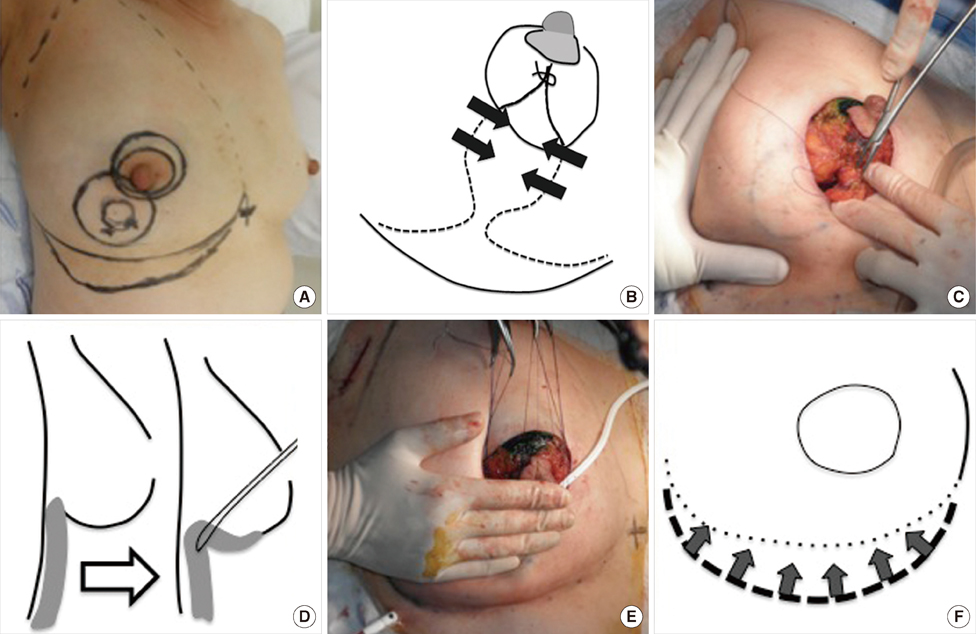
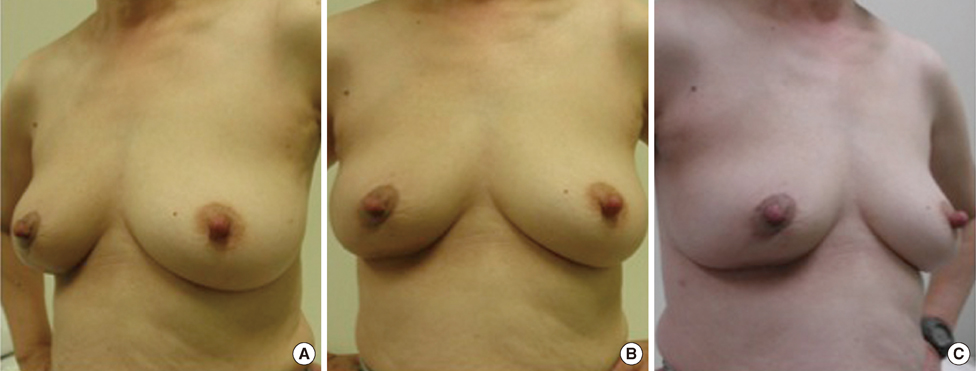
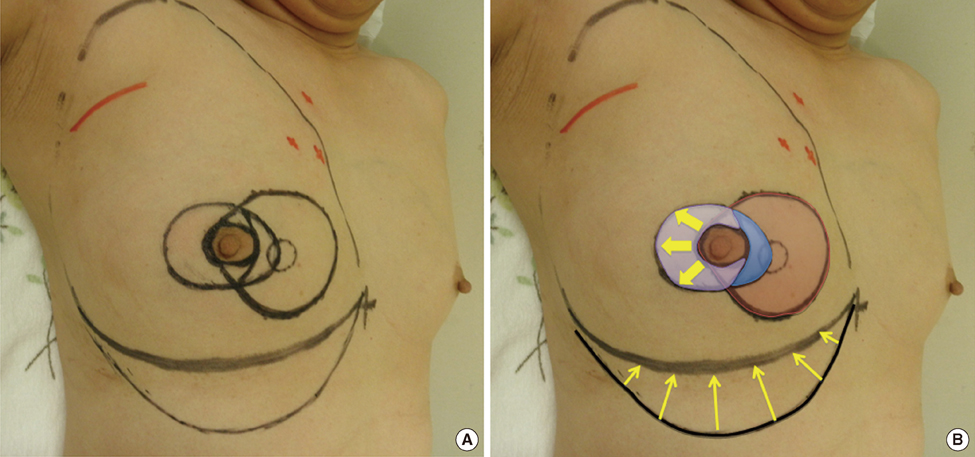
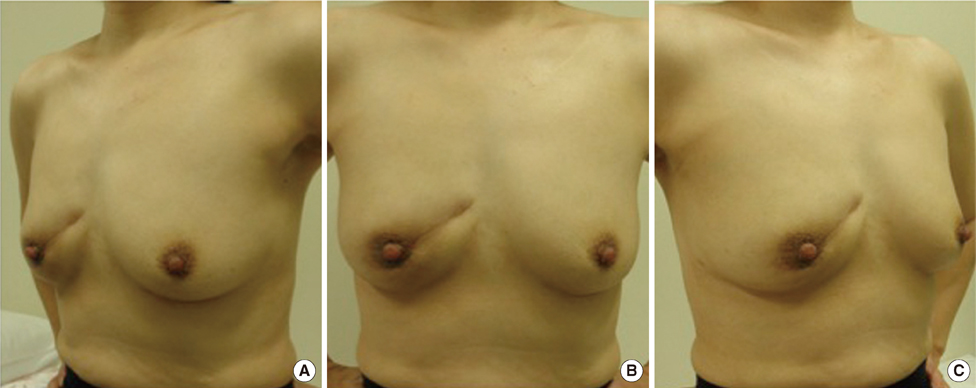
- An abdominal advancement flap (AAF) is a flap that pulls the elevated abdominal skin up and creates the shape of the inferior portion of the breast by making a neo-inframammary fold. Seven patients underwent remodeling using an AAF or a method combining an AAF with other volume displacement techniques after partial mastectomy. The excision volume ranged from 15% to 35%. AAF with only mobilization of the gland flaps was performed in two cases, with lateral mammoplasty in one case, with the round block technique (RBT) in one case, with a modified RBT in one case, and with medial mammoplasty in two cases. Although one patient treated with a RBT had a partial blood-flow insufficiency of the nipple-areola complex, it improved with conservative treatment. The cosmetic results were found to be excellent in three cases, good in three, and fair in one case.
MeSH Terms
Figure
Reference
-
1. Bulstrode NW, Shrotria S. Prediction of cosmetic outcome following conservative breast surgery using breast volume measurements. Breast. 2001; 10:124–126.
Article2. McCulley SJ, Macmillan RD. Planning and use of therapeutic mammoplasty: Nottingham approach. Br J Plast Surg. 2005; 58:889–901.3. Kronowitz SJ, Hunt KK, Kuerer HM, Strom EA, Buchholz TA, Ensor JE, et al. Practical guidelines for repair of partial mastectomy defects using the breast reduction technique in patients undergoing breast conservation therapy. Plast Reconstr Surg. 2007; 120:1755–1768.
Article4. Clough KB, Ihrai T, Oden S, Kaufman G, Massey E, Nos C. Oncoplastic surgery for breast cancer based on tumour location and a quadrant-per-quadrant atlas. Br J Surg. 2012; 99:1389–1395.
Article5. Lewis JR Jr. Use of a sliding flap from the abdomen to provide cover in breast reconstructions. Plast Reconstr Surg. 1979; 64:491–497.
Article6. Ryan JJ. A lower thoracic advancement flap in breast reconstruction after mastectomy. Plast Reconstr Surg. 1982; 70:153–160.
Article7. Delay E, Jorquera F, Pasi P, Gratadour AC. Autologous latissimus breast reconstruction in association with the abdominal advancement flap: a new refinement in breast reconstruction. Ann Plast Surg. 1999; 42:67–75.
Article8. Leal PR, de Souza AF. Breast reconstruction by expansion and advancement of the upper abdominal flap. Aesthetic Plast Surg. 1997; 21:175–179.
Article9. Fitoussi A, Couturaud B, Salmon RJ. Abdominal advancement flap and the IMF. In : Fitoussi A, Berry MG, Couturaud B, Salmon RJ, editors. Oncoplastic and Reconstructive Surgery for Breast Cancer: the Institut Curie Experience. Berlin: Springer;2009. p. 48–52.10. Harris JR, Levene MB, Svensson G, Hellman S. Analysis of cosmetic results following primary radiation therapy for stages I and II carcinoma of the breast. Int J Radiat Oncol Biol Phys. 1979; 5:257–261.
Article11. Clough KB, Kaufman GJ, Nos C, Buccimazza I, Sarfati IM. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann Surg Oncol. 2010; 17:1375–1391.
Article12. Ogawa T, Hanamura N, Yamashita M, Ri Y, Kuriyama N, Isaji S. Usefulness of breast-volume replacement using an inframammary adipofascial flap after breast-conservation therapy. Am J Surg. 2007; 193:514–518.
Article13. Ogawa T, Hanamura N, Yamashita M, Kimura H, Kashikura Y. Long-term results of breast volume replacement using an inframammary adipofascial flap after breast-conserving surgery. Breast Cancer. Epub 2011 Jun 28. DOI: http://dx.doi.org/10.1007/s12282-011-0285-2.
Article14. Aljarrah A, Nos C, Nasr R, Clough KB, Bats AS, Lecuru F. Updated follow-up of patients treated with the oncoplastic "Crescent" technique for breast cancer. Breast. 2012; 21:475–479.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oncoplastic Breast Surgery
- Oncoplastic Technique Combining an Adipofascial Flap with an Extended Glandular Flap for the Breast-Conserving Reconstruction of Small Dense Breasts
- Surgical Techniques for Personalized Oncoplastic Surgery in Breast Cancer Patients with Small- to Moderate-Sized Breasts (Part 2): Volume Replacement
- Surgical Techniques for Personalized Oncoplastic Surgery in Breast Cancer Patients with Small- to Moderate-Sized Breasts (Part 1): Volume Displacement
- Usefulness of Oncoplastic Volume Replacement Techniques after Breast Conserving Surgery in Small to Moderate-sized Breasts