Infect Chemother.
2013 Jun;45(2):202-210. 10.3947/ic.2013.45.2.202.
Impact of Methicillin-Resistance on Mortality in Children and Neonates with Staphylococcus aureus Bacteremia: A Meta-analysis
- Affiliations
-
- 1Office of Health Technology Evaluation, National Evidence-based Healthcare Collaborating Agency, Seoul, Korea. lsm@neca.re.kr
- 2College of Nursing Yonsei University, Seoul, Korea.
- 3Division of Infectious Diseases, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. krpeck@skku.edu
- 4Institute of Nursing Policy and Research, College of Nursing Yonsei University, Seoul, Korea.
- KMID: 2285001
- DOI: http://doi.org/10.3947/ic.2013.45.2.202
Abstract
- BACKGROUND
Staphylococcus aureus bacteremia (SAB) is the Staphylococcal infections in blood, one of the most common and fatal bacterial infectious diseases worldwide in adults as well as children or neonates. Recently, some studies have yielded inconsistent findings about the association between methicillin-resistance and mortality in patients with SAB. We performed a meta-analysis to assess the impact of methicillin-resistance on mortality in children or neonates with S. aureus bacteremia.
MATERIALS AND METHODS
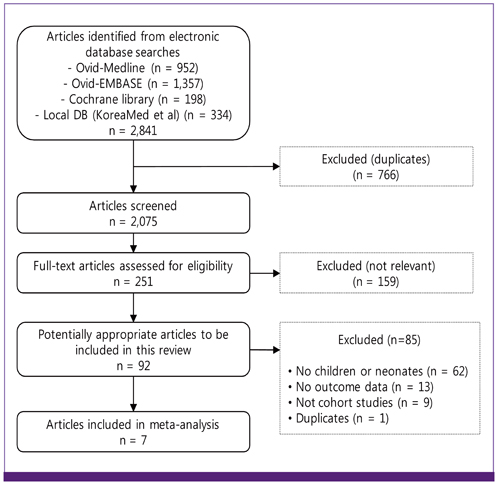
We searched using electronic databases such as Ovid-Medline, EMBASE-Medline, and Cochrane Library, as well as five local databases for published studies during the period of 1 January 2000 to 15 September 2011. Two reviewers independently selected articles in accordance with predetermined criteria and extracted prespecified data based on standardized forms. All cohort studies, which compared in-hospital mortality or SAB-related mortality in children and neonates with methicillin-resistant S. aureus (MRSA) infection to those with methicillin-susceptible S. aureus (MSSA), were included. We conducted meta-analysis using the fixed-effect model to obtain pooled estimates of effect.
RESULTS
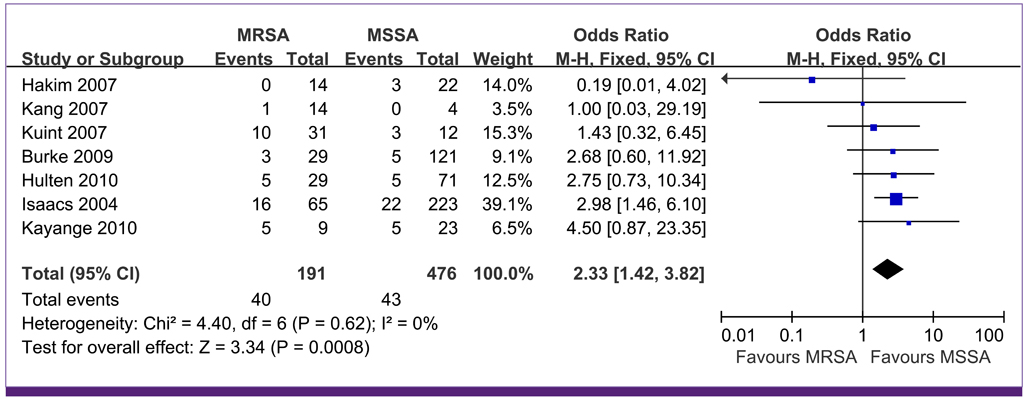
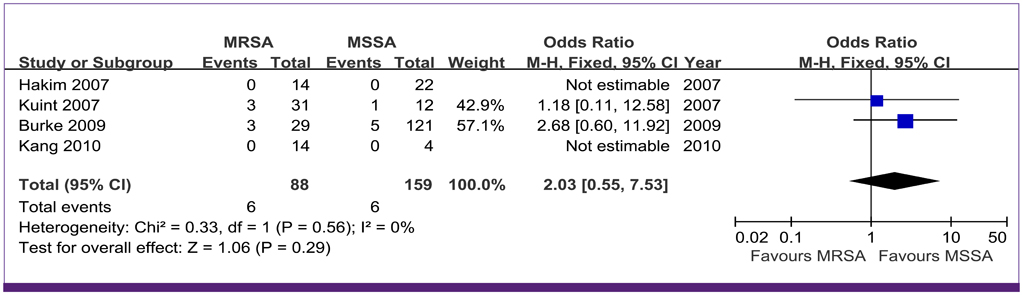
Of 2,841 screened studies, seven cohort studies were finally selected for analysis. In children or neonates, MRSA bacteremia was associated with a higher mortality compared with MSSA bacteremia (pooled odds ratio [OR] 2.33, P = 0.0008, 95% confidence interval [CI] 1.42 to 3.82, I2 = 0%). Four studies reported SAB-related mortality, the pooled OR of these studies was 2.03 (P = 0.29, 95% CI 0.55 to 7.53, I2 = 0%). A significant increase in mortality associated with methicillin resistance was found in the subgroup analyses of the studies with only neonates (OR: 2.66, 95% CI: 1.46 to 4.85, P = 0.001), prospectively design ones (OR: 3.20, 95% CI: 1.66 to 6.15, P = 0.0005,), the larger studies (OR: 2.89, 95% CI: 1.62 to 5.16, P = 0.0003) and the higher quality studies (OR: 2.76, 95% CI: 1.50 to 5.06, P = 0.001).
CONCLUSIONS
MRSA bacteremia is associated with increased mortality compared with MSSA bacteremia in children or neonates. Due to limited studies for mortality in children or neonates with SAB, further research is needed to evaluate the impact of methicillin resistance on mortality in those populations.
MeSH Terms
Figure
Reference
-
1. Laupland KB, Church DL, Mucenski M, Sutherland LR, Davies HD. Population-based study of the epidemiology of and the risk factors for invasive Staphylococcus aureus infections. J Infect Dis. 2003. 187:1452–1459.
Article2. Brumfitt W, Hamilton-Miller JM. The worldwide problem of methicillin-resistant Staphylococcus aureus. Drugs Exp Clin Res. 1990. 16:205–214.3. Naimi TS, LeDell KH, Como-Sabetti K, Borchardt SM, Boxrud DJ, Etienne J, Johnson SK, Vandenesch F, Fridkin S, O'Boyle C, Danila RN, Lynfield R. Comparison of community-and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003. 290:2976–2984.
Article4. Kaech C, Elzi L, Sendi P, Frei R, Laifer G, Bassetti S, Fluckiger U. Course and outcome of Staphylococcus aureus bacteremia: a retrospective analysis of 308 episodes in a Swiss tertiary-care centre. Clin Microbiol Infect. 2006. 12:345–352.
Article5. Kern WV. Management of Staphylococcus aureus bacteremia and endocarditis: progress and challenges. Curr Opin Infect Dis. 2010. 23:346–358.
Article6. Whitby M, McLaws ML, Berry G. Risk of death from methicillin-resistant Staphylococcus aureus bacteraemia: a meta-analysis. Med J Aust. 2001. 175:264–267.
Article7. Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin Infect Dis. 2003. 36:53–59.
Article8. Herold BC, Immergluck LC, Maranan MC, Lauderdale DS, Gaskin RE, Boyle-Vavra S, Leitch CD, Daum RS. Community-acquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA. 1998. 279:593–598.
Article9. Khairulddin N, Bishop L, Lamagni TL, Sharland M, Duckworth G. Emergence of methicillin resistant Staphylococcus aureus (MRSA) bacteraemia among children in England and Wales, 1990-2001. Arch Dis Child. 2004. 89:378–379.
Article10. Chuang YY, Huang YC, Lee CY, Lin TY, Lien R, Chou YH. Methicillin-resistant Staphylococcus aureus bacteraemia in neonatal intensive care units: an analysis of 90 episodes. Acta Paediatr. 2004. 93:786–790.
Article11. Purcell K, Fergie J. Epidemic of community-acquired methicillin-resistant Staphylococcus aureus infections: a 14-year study at Driscoll Children's Hospital. Arch Pediatr Adolesc Med. 2005. 159:980–985.
Article12. Hakim H, Mylotte JM, Faden H. Morbidity and mortality of Staphylococcal bacteremia in children. Am J Infect Control. 2007. 35:102–105.
Article13. Burke RE, Halpern MS, Baron EJ, Gutierrez K. Pediatric and neonatal Staphylococcus aureus bacteremia: epidemiology, risk factors, and outcome. Infect Control Hosp Epidemiol. 2009. 30:636–644.
Article14. Isaacs D, Fraser S, Hogg G, Li HY. Staphylococcus aureus infections in Australasian neonatal nurseries. Arch Dis Child Fetal Neonatal Ed. 2004. 89:F331–F335.15. Kuint J, Barzilai A, Regev-Yochay G, Rubinstein E, Keller N, Maayan-Metzger A. Comparison of community-acquired methicillin-resistant Staphylococcus aureus bacteremia to other staphylococcal species in a neonatal intensive care unit. Eur J Pediatr. 2007. 166:319–325.
Article16. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986. 7:177–188.
Article17. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Accessed 20 August 2012. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003. 327:557–560.
Article19. Hogg RV, Tanis EA. Probability and Statistical Inference. 1988. 3rd ed. New York: Macmillan.20. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997. 315:629–634.
Article21. Begg CB, Manzumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994. 50:1088–1101.
Article22. Hultén KG, Kaplan SL, Lamberth LB, Slimp K, Hammerman WA, Carrillo-Marquez M, Starke JR, Versalovic J, Mason EO Jr. Hospital-acquired Staphylococcus aureus infections at Texas Children's Hospital, 2001-2007. Infect Control Hosp Epidemiol. 2010. 31:183–190.
Article23. Kayange N, Kamugisha E, Mwizamholya DL, Jeremiah S, Mshana SE. Predictors of positive blood culture and deaths among neonates with suspected neonatal sepsis in a tertiary hospital, Mwanza-Tanzania. BMC Pediatr. 2010. 10:39.24. Kang HC, Lee KC, Kim SS, Park JO, Kim CH. Staphylococcal infection in the neonatal intensive care unit. J Korean Soc Neonatol. 2007. 14:215–220.25. Easterbrook PJ, Berlin JA, Gopalan R, Matthews DR. Publication bias in clinical research. Lancet. 1991. 337:867–872.
Article26. Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions Version 5.0.2. [Updated September 2009]. 2009. Accessed 20 August 2012. The Cochrane Collaboration;Available at: www.mrc-bsu.cam.ac.uk/cochrane/handbook502/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microbiological and genotypic factors affecting mortality in methicillin-resistant Staphylococcus aureus bacteremia
- Clinical Observation on Staphylococcus aureus Bacteremia of Community Hospital
- The risk factors and prognosis of methicillin-resistant staphylococcus aureus bacteremia: focus on nosocomial acquisition
- A statistical analysis of methicillin-resistant staphylococcus aureus
- Community-acquired Methicillin-resistant Staphylococcus aureus Bacteremia Complicated by Acute Cholecystitis