Infect Chemother.
2014 Sep;46(3):209-215. 10.3947/ic.2014.46.3.209.
Aspergillus Tracheobronchitis and Influenza A Co-infection in a Patient with AIDS and Neutropenia
- Affiliations
-
- 1Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. eunjeong.joo@samsung.com
- 2Department of Pathology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2284980
- DOI: http://doi.org/10.3947/ic.2014.46.3.209
Abstract
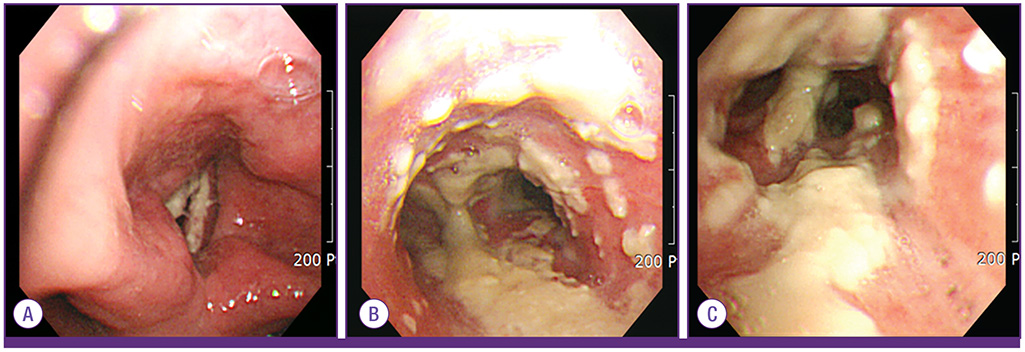
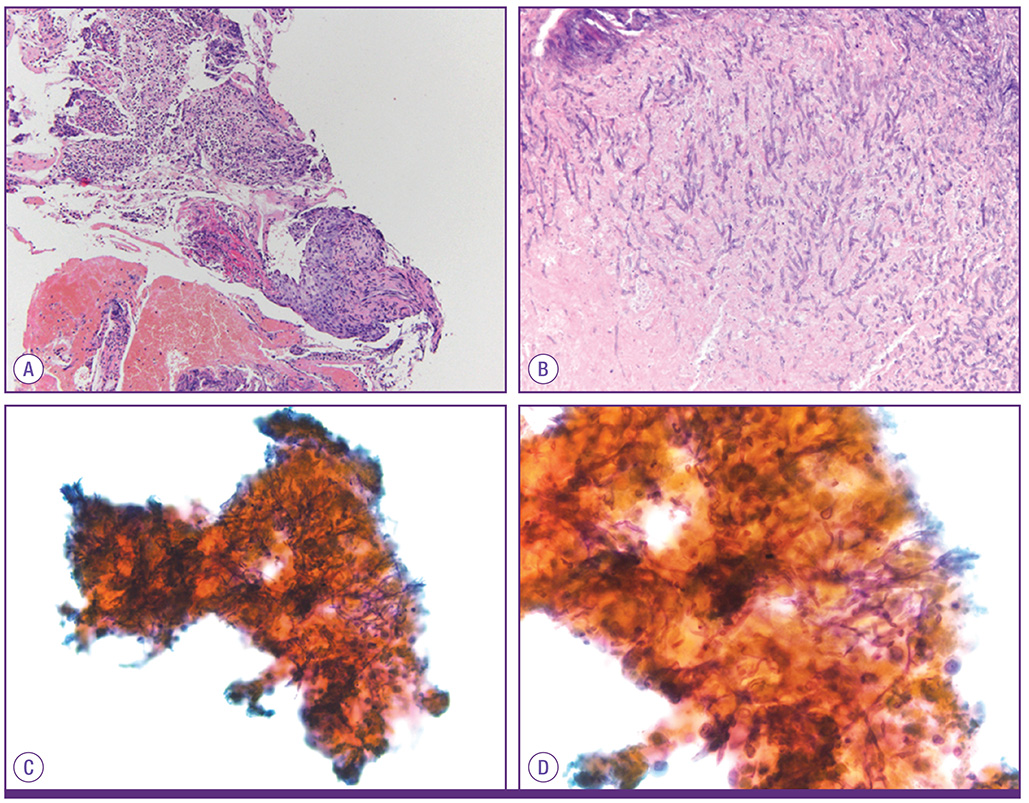
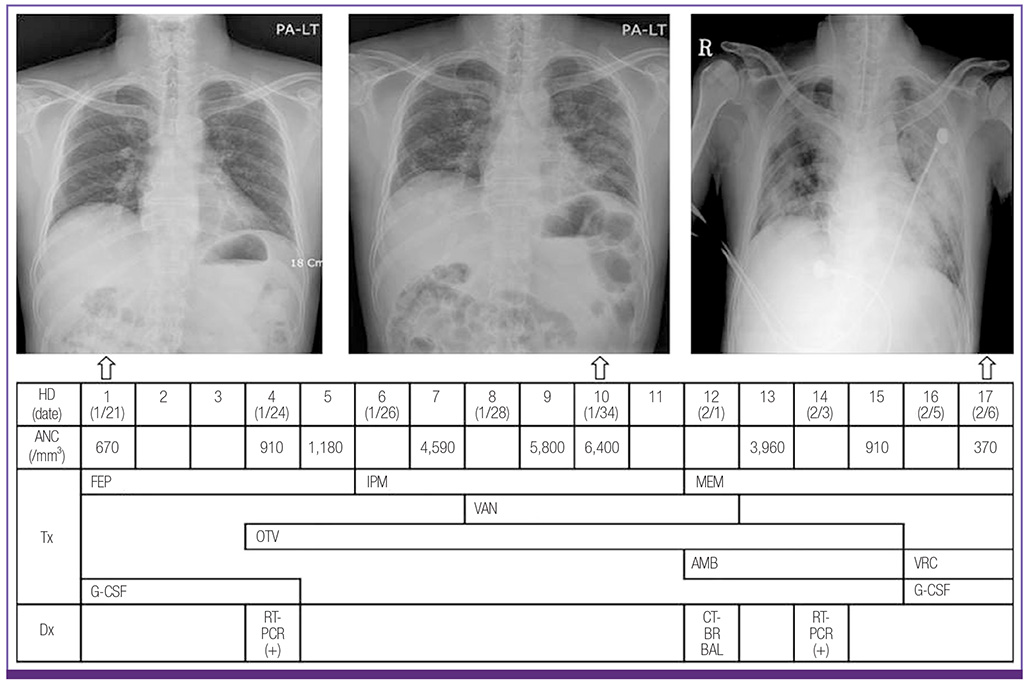
- Aspergillus tracheobronchitis (AT), an unusual form of invasive pulmonary aspergillosis (IPA), is characterized by pseudomembrane formation, ulcer or obstruction that is predominantly confined to tracheobronchial tree. Hematologic malignancies, neutropenia, solid organ transplantation, chronic corticosteroid therapy and acquired immunodeficiency syndrome (AIDS) are known to be major predisposing conditions. However, since the introduction of highly active antiretroviral therapy, there is only one reported case of AT in AIDS patient. After pandemic of influenza A/H1N1 2009, there are several reports of IPA in patient with influenza and most of them received corticosteroid or immunosuppressive therapy before the development of IPA. We present a 45 year-old AIDS patient with influenza A infection who developed pseudomembranous AT without corticosteroid use or immunosuppressive therapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Segal BH. Aspergillosis. N Engl J Med. 2009; 360:1870–1884.
Article2. Denning DW. Commentary: unusual manifestations of aspergillosis. Thorax. 1995; 50:812–813.
Article3. Fernández-Ruiz M, Silva JT, San-Juan R, de Dios B, García-Luján R, López-Medrano F, Lizasoain M, Aguado JM. Aspergillus tracheobronchitis: report of 8 cases and review of the literature. Medicine (Baltimore). 2012; 91:261–273.4. Denning DW, Follansbee SE, Scolaro M, Norris S, Edelstein H, Stevens DA. Pulmonary aspergillosis in the acquired immunodeficiency syndrome. N Engl J Med. 1991; 324:654–662.
Article5. Holding KJ, Dworkin MS, Wan PC, Hanson DL, Klevens RM, Jones JL, Sullivan PS. Aspergillosis among people infected with human immunodeficiency virus: incidence and survival. Adult and Adolescent Spectrum of HIV Disease Project. Clin Infect Dis. 2000; 31:1253–1257.
Article6. Wauters J, Baar I, Meersseman P, Meersseman W, Dams K, De Paep R, Lagrou K, Wilmer A, Jorens P, Hermans G. Invasive pulmonary aspergillosis is a frequent complication of critically ill H1N1 patients: a retrospective study. Intensive Care Med. 2012; 38:1761–1768.
Article7. Dal Conte I, Riva G, Obert R, Lucchini A, Bechis G, De Rosa G, Gioannini P. Tracheobronchial aspergillosis in a patient with AIDS treated with aerosolized amphotericin B combined with itraconazole. Mycoses. 1996; 39:371–374.
Article8. Kemper CA, Hostetler JS, Follansbee SE, Ruane P, Covington D, Leong SS, Deresinski SC, Stevens DA. Ulcerative and plaque-like tracheobronchitis due to infection with Aspergillus in patients with AIDS. Clin Infect Dis. 1993; 17:344–352.
Article9. Pervez NK, Kleinerman J, Kattan M, Freed JA, Harris MB, Rosen MJ, Schwartz IS. Pseudomembranous necrotizing bronchial aspergillosis. A variant of invasive aspergillosis in a patient with hemophilia and acquired immune deficiency syndrome. Am Rev Respir Dis. 1985; 131:961–963.10. Antinori S, Ridolfo AL, Galimberti L, Milazzo L, Giuliani G, Ferraris L, Maruzzi M, Corbellino M. Usefulness of serial determination of Aspergillus galactomannan in the diagnosis and management of invasive aspergillosis in an AIDS patient with non-Hodgkin lymphoma. Mycoses. 2011; 54:e885–e888.
Article11. Hage CA, Goldman M, Wheat LJ. Mucosal and invasive fungal infections in HIV/AIDS. Eur J Med Res. 2002; 7:236–241.12. Choi JK, No JH, Lee BH, Yun JS, Kim SH, Kwon JC, Hong JH, Lee GJ, Park SH, Choi SM, Lee DG, Choi JH, Yoo JH. Invasive tracheobronchial aspergillosis : case reports and a literature review. Infect Chemother. 2011; 43:76–81.
Article13. Boots RJ, Paterson DL, Allworth AM, Faoagali JL. Successful treatment of post-influenza pseudomembranous necrotising bronchial aspergillosis with liposomal amphotericin, inhaled amphotericin B, gamma interferon and GM-CSF. Thorax. 1999; 54:1047–1049.
Article14. Kim SH, Kim MN, Lee SO, Choi SH, Kim YS, Woo JH, Lim CM, Koh Y, Hong SB. Fatal pandemic influenza A/H1N1 infection complicated by probable invasive pulmonary aspergillosis. Mycoses. 2012; 55:189–192.
Article15. Tasci S, Glasmacher A, Lentini S, Tschubel K, Ewig S, Molitor E, Sauerbruch T, Lüderitz B, Rabe C. Pseudomembranous and obstructive Aspergillus tracheobronchitis - optimal diagnostic strategy and outcome. Mycoses. 2006; 49:37–42.
Article16. Thonar B, Yoder M, Cleaves C. Not your typical chronic obstructive pulmonary disease exacerbation: Aspergillus tracheobronchitis in a nonclassical immunocompromised host. South Med J. 2010; 103:361–365.
Article17. Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Segal BH, Steinbach WJ, Stevens DA, van Burik JA, Wingard JR, Patterson TF. Infectious Diseases Society of America. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008; 46:327–360.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pseudomembranous Aspergillus Tracheobronchitis in a Patient with Diabetes Mellitus
- Pseudomembranous Aspergillus Tracheobronchitis: Case Report of a Rare Manifestation of Airway Invasive Aspergillosis
- Airway Obstruction and Respiratory Failure Due to Aspergillus Tracheobronchitis
- Death due to Aspergillus Tracheobronchitis: An Autopsy Case
- A Case of Severe Pseudomembranous Tracheobronchitis Complicated by Co-infection of Influenza A (H1N1) and Staphylococcus aureus in an Immunocompetent Patient