Ewha Med J.
2011 Sep;34(2):55-59. 10.12771/emj.2011.34.2.55.
Acute Pancreatitis Caused by Dyslipidemia
- Affiliations
-
- 1Department of Internal Medicine, Daerim Saint Mary's Hospital, Seoul, Korea. mybestdoctor@paran.com
- 2Department of Laboratory Medicine, Daerim Saint Mary's Hospital, Seoul, Korea.
- KMID: 2283971
- DOI: http://doi.org/10.12771/emj.2011.34.2.55
Abstract
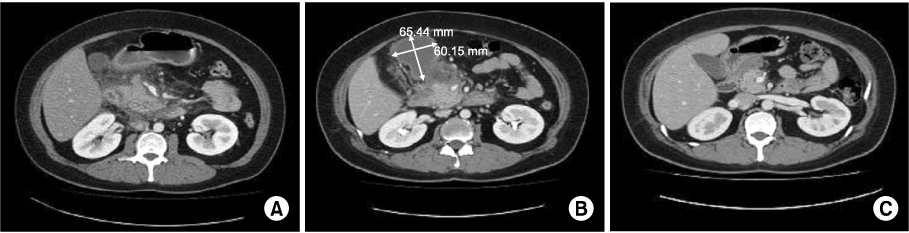
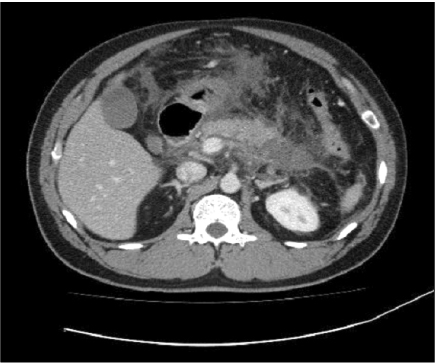
- Hyperlipidemia can be a cause of acute pancreatitis. For example, dyslipidemia classified Fredrickson/WHO classification type I, V can induce acute pancreatitis spontaneously. Secondary hyperlipidemia (DM, alcohol, estrogen, etc.) also can induce acute pancreatitis. High serum amylase level and triglyceride level are hall markers of diagnosis. But lactescent serum interferes with accurate laboratory analysis of amylase. Serum amylase was normal or low in 50% of cases. Clinical course and treatment are similar with other causes of acute pancreatitis. Lipoprotein electrophoresis helps classify dyslipidemia by Fredrickson/WHO classification. In some cases, to prevent hyperlipidemic pancreatitis, serum triglyceride should be lower than 500 mg/dl. We report two cases of acute pancreatitis caused by dyslipidemia.
Keyword
MeSH Terms
Figure
Reference
-
1. Yadav D, Pitchumoni CS. Issues in hyperlipidemic pancreatitis. J Clin Gastroenterol. 2003. 36:54–62.
Article2. Kim BK, Kim J, Chang WC, Yoo KH, Shin YG, Chung CH. Recurrent acute pancreatitis in a patient with type iib hyperlipoproteinemia: a case report and review of the literature in Korea. Yonsei Med J. 2006. 47:144–147.
Article3. Kim YJ, Kim HJ, Kim HC, Kim SJ, Park SH. A case of acute hyperlipidemic pancreatitis in a patient suspected of familial combined hyperlipidemia. Korean J Med. 2005. 69:197–201.4. Kim YK, Kim HJ, Kim BH, Chang YW, Chang R. A case of acute pancreatitis with secondary hyperlipidemia. Korean J Gastroenterol. 1991. 23:993–998.5. Cho CS, Lee SH, Hong YS, Park DJ, Kim HY. A case of chylomicronemia syndrome in systemic lupus erythematosus. Korean J Med. 1993. 45:659–663.6. Speck L. Fall von lipamia. Arch Verin Wissenschaftl Heilkunde. 1865. 1:232.7. Fortson MR, Freedman SN, Webster PD 3rd. Clinical asscessment of hyperlipidemic pancreatitis. Am J Gastroenterol. 1995. 90:2134–2139.8. Havel RJ. Pathogenesis, differentiation and management of hypertriglyvemia. Adv Intern Med. 1969. 15:117.9. Gan SI, Edwards AL, Symonds CJ, Beck PL. Hypertriglyceridemia-induced pancreatitis. World J Gastroenterol. 2006. 12:7197–7202.10. Lesser PB, Warshaw AL. Diagnosis of pancreatitis masked by hyperlipidemia. Ann Intern Med. 1975. 82:795–798.11. Kim JQ, Song JH. Lipids. The Korean Society for Laboratory Medicine. Laboratory Medicine. 2001. 3rd ed. Seoul: Korea Medicine;65.12. Brunzell JD. Hyperytriglyceridemia. N Engl J Med. 2007. 357:1009–1017.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Pancreatitis associated with Acute Hepatitis A in an Old Aged Patient
- A Case of Acute Pancreatitis Caused by Bortezomib in a Patient with Multiple Myeloma
- A case of acute pancreatitis caused by hyperparathyroidism
- A Case Report of Acute Pancreatitis Caused by Mycoplasma Pneumoniae Infection
- Acute Pancreatitis caused by Hemobilia after Percutaneous Liver Biopsy