Clin Nutr Res.
2013 Jan;2(1):1-11. 10.7762/cnr.2013.2.1.1.
Evaluation of Nutrient Intake in Early Post Kidney Transplant Recipients
- Affiliations
-
- 1Department of Food Service and Nutritional Care, Seoul National University Hospital, Seoul 110-744, Korea. nutri@snuh.org
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul 110-744, Korea.
- KMID: 2279709
- DOI: http://doi.org/10.7762/cnr.2013.2.1.1
Abstract
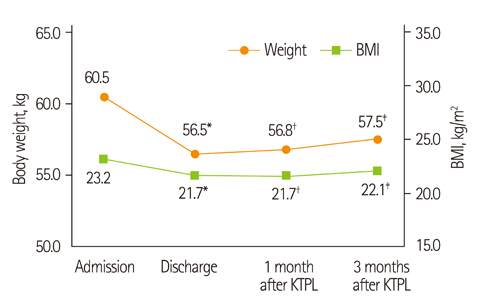
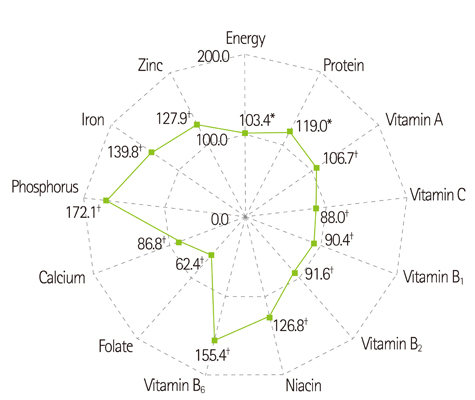
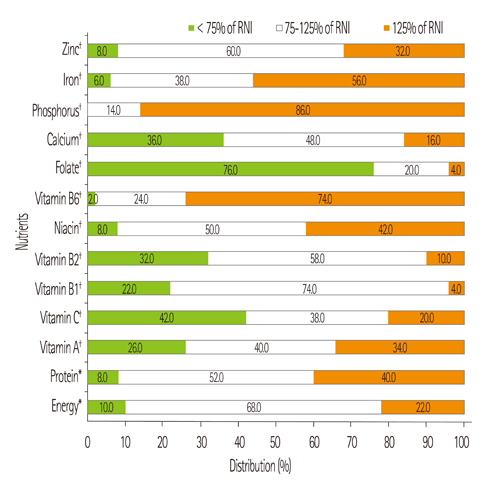
- The purpose of our study was to evaluate the dietary intake of kidney transplant recipients (KTRs) and assess oral intake related nutrition problems. Fifty patients who had undergone kidney transplantation were included: 24 males, 26 females. The mean age was 46.8 +/- 11.2 years, height was 161.3 +/- 8.3 cm, and body weight was 60.5 +/- 8.7 kg. We conducted nutrition education based on the diet guideline for KTRs (energy 32 kcal/kg of ideal body weight [IBW], protein 1.3 g/kg of IBW) and neutropenic diet guideline before discharge. Dietary intake of the patients at 1 month after transplantation was investigated by 3-day food records. Body weight and laboratory values for nutritional status and graft function were also collected. Body weight was significantly decreased from admission to discharge. Body weight from discharge to 1 month and 3 months after transplantation was increased but was not significant. Biochemical measurements were generally improved but the number of patients with hypophosphatemia increased. The daily dietary intake of energy and protein was adequate (33.1 kcal/kg, 1.5 g/kg, respectively). However, the dietary intake of calcium, folate, and vitamin C did not meet the Korean Recommended Nutrient Intake of vitamins and minerals (86.8%, 62.4%, and 88.0%, respectively). Patients with low intake of calcium, folate, and vitamin C presented low intake in milk and dairy products, vegetables, and fruits, and these foods were related to restricted food items in neutropenic diet. More attention should be paid on improving quality of diet, and reconsideration of present neutropenic diet guideline is necessary. These results can be used to establish evidence-based medical nutrition therapy guideline for KTRs.
MeSH Terms
Figure
Reference
-
1. Ministry of Health and Welfare. Korean Network for Organ Sharing. Annual report of the transplant 2011. Seoul: Korean Network for Organ Sharing;2012.2. Kim MH, Kim MS, Kwon OJ, Kang CM. Comparison of quality of life between kidney transplant patients and dialysis patients. J Korean Soc Transplant. 2009; 23:65–70.
Article3. Laupacis A, Keown P, Pus N, Krueger H, Ferguson B, Wong C, Muirhead N. A study of the quality of life and cost-utility of renal transplantation. Kidney Int. 1996; 50:235–242.
Article4. Favi E, Salerno MP, Romagnoli J, Castagneto M, Citterio F. Significant improvement in patient survival after renal transplantation in the last decade. Transplant Proc. 2011; 43:285–287.
Article5. Wang K, Liu QZ. Effect analysis of 1-year posttransplant body mass index on chronic allograft nephropathy in renal recipients. Transplant Proc. 2011; 43:2592–2595.
Article6. Armstrong KA, Campbell SB, Hawley CM, Nicol DL, Johnson DW, Isbel NM. Obesity is associated with worsening cardiovascular risk factor profiles and proteinuria progression in renal transplant recipients. Am J Transplant. 2005; 5:2710–2718.
Article7. Teplan V, Valkovsky I, Teplan V Jr, Stollova M, Vyhnanek F, Andel M. Nutritional consequences of renal transplantation. J Ren Nutr. 2009; 19:95–100.
Article8. Bia M, Adey DB, Bloom RD, Chan L, Kulkarni S, Tomlanovich S. KDOQI US commentary on the 2009 KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Kidney Dis. 2010; 56:189–218.
Article9. Lopes IM, Martín M, Errasti P, Martínez JA. Benefits of a dietary intervention on weight loss, body composition, and lipid profile after renal transplantation. Nutrition. 1999; 15:7–10.
Article10. Martins C, Pecoits-Filho R, Riella MC. Nutrition for the post-renal transplant recipients. Transplant Proc. 2004; 36:1650–1654.
Article11. Beto JA, Bansal VK. Medical nutrition therapy in chronic kidney failure: integrating clinical practice guidelines. J Am Diet Assoc. 2004; 104:404–409.
Article12. Byham-Gray L, Wiesen K. American Dietetic Association Renal Practice Group. National Kidney Foundation Council on Renal Nutrition. A clinical guide to nutrition care in kidney disease. Chicago, IL: American Dietetic Association;2004.13. The Korean Dietetic Association. Manual of medical nutrition therapy. 2nd ed. Seoul: Kyung Hee;1999.14. The Korean Nutrition Society. Dietary reference intakes for Koreans. 1st rev. Seoul: Hanareum;2010.15. Leavey SF, McCullough K, Hecking E, Goodkin D, Port FK, Young EW. Body mass index and mortality in 'healthier' as compared with 'sicker' haemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2001; 16:2386–2394.
Article16. Odamaki M, Furuya R, Yoneyama T, Nishikino M, Hibi I, Miyaji K, Kumagai H. Association of the serum leptin concentration with weight loss in chronic hemodialysis patients. Am J Kidney Dis. 1999; 33:361–368.
Article17. Johnson DW, Isbel NM, Brown AM, Kay TD, Franzen K, Hawley CM, Campbell SB, Wall D, Griffin A, Nicol DL. The effect of obesity on renal transplant outcomes. Transplantation. 2002; 74:675–681.
Article18. Djukanović L, Lezaić V, Blagojević R, Radivojević D, Stosović M, Jovanović N, Ristić S, Simić-Ogrizović S. Co-morbidity and kidney graft failure-two main causes of malnutrition in kidney transplant patients. Nephrol Dial Transplant. 2003; 18:Suppl 5. v68–v70.19. Rettkowski O, Wienke A, Hamza A, Osten B, Fornara P. Low body mass index in kidney transplant recipients: risk or advantage for long-term graft function? Transplant Proc. 2007; 39:1416–1420.
Article20. Netto MC, Alves-Filho G, Mazzali M. Nutritional status and body composition in patients early after renal transplantation. Transplant Proc. 2012; 44:2366–2368.
Article21. Nishi S, Gejyo F, Saito K, Nakagawa Y, Takahashi K. Diet therapy after kidney transplantation: a comparative debate between Japan and western countries. Contrib Nephrol. 2007; 155:82–89.22. Jones CH, Akbani H, Croft DC, Worth DP. The relationship between serum albumin and hydration status in hemodialysis patients. J Ren Nutr. 2002; 12:209–212.
Article23. Coroas AS, de Oliveira JG, Sampaio SM, Tavares IC, Pestana M, Almeida MD. Postrenal transplantation body composition: different evolution depending on gender. J Ren Nutr. 2007; 17:151–156.
Article24. Chadban S, Chan M, Fry K, Patwardhan A, Ryan C, Trevillian P, Westgarth F. CARI. The CARI guidelines. Protein requirement in adult kidney transplant recipients. Nephrology (Carlton). 2010; 15:Suppl 1. S68–S71.25. Han SS, Hwang JH, Oh YJ, Cha RH, Ahn C, Kim YS. Change in body compositions of Asian recipients after kidney transplantation. J Korean Med Sci. 2012; 27:1182–1187.
Article26. Ministry of Health and Welfare, Korea Centers for Disease Control & Prevention. Korea health statistics 2010: Korea National Health and Nutrition Examination Survey (KNHANES V-1) 2010. Seoul: Ministry of Health and Welfare, Korea Centers for Disease Control & Prevention;2011.27. Pichette V, Bonnardeaux A, Prudhomme L, Gagné M, Cardinal J, Ouimet D. Long-term bone loss in kidney transplant recipients: a cross-sectional and longitudinal study. Am J Kidney Dis. 1996; 28:105–114.
Article28. Coco M, Glicklich D, Faugere MC, Burris L, Bognar I, Durkin P, Tellis V, Greenstein S, Schechner R, Figueroa K, McDonough P, Wang G, Malluche H. Prevention of bone loss in renal transplant recipients: a prospective, randomized trial of intravenous pamidronate. J Am Soc Nephrol. 2003; 14:2669–2676.
Article29. Chan M, Patwardhan A, Ryan C, Trevillian P, Chadban S, Westgarth F, Fry K. Caring for Australasians with Renal Impairment. Dietitians Association of Australia. Evidence-based guidelines for the nutritional management of adult kidney transplant recipients. J Ren Nutr. 2011; 21:47–51.
Article30. Heaf J, Jakobsen U, Tvedegaard E, Kanstrup IL, Fogh-Andersen N. Dietary habits and nutritional status of renal transplant patients. J Ren Nutr. 2004; 14:20–25.
Article31. Selhub J, Jacques PF, Wilson PW, Rush D, Rosenberg IH. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. JAMA. 1993; 270:2693–2698.
Article32. Arnadottir M, Hultberg B, Vladov V, Nilsson-Ehle P, Thysell H. Hyperhomocysteinemia in cyclosporine-treated renal transplant recipients. Transplantation. 1996; 61:509–512.
Article33. Han YH, Yon M, Hyun TH. Folate intake estimated with an updated database and its association to blood folate and homocysteine in Korean college students. Eur J Clin Nutr. 2005; 59:246–254.
Article34. Hsieh MM, Everhart JE, Byrd-Holt DD, Tisdale JF, Rodgers GP. Prevalence of neutropenia in the U.S. population: age, sex, smoking status, and ethnic differences. Ann Intern Med. 2007; 146:486–492.
Article35. French MR, Levy-Milne R, Zibrik D. A survey of the use of low microbial diets in pediatric bone marrow transplant programs. J Am Diet Assoc. 2001; 101:1194–1198.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Concept Analysis of Compliance in Kidney Transplant Recipient Including Compliance with Immunosuppressive Medication
- Surgical Complications are Major Problems Concerning Overseas Kidney Transplantation in Comparison Study with Domestic Deceased Donor Kidney Transplantation
- Change of Bone Mineral Density after Kidney Transplantation and Factors Influencing Post-transplant Bone Mineral Density Loss
- A Prediction Model Development on Quality of Life in Kidney Transplant Recipients
- Cytomegalovirus infection and risk of new-onset diabetes after transplantation: a retrospective analysis