Korean J Pediatr Infect Dis.
2013 Apr;20(1):1-8.
Clinical Manifestations of Salmonellosis in Children during the last 12 Years: A Single Institution Experience
- Affiliations
-
- 1Department of Pediatrics, CHA Bundang Medical Center, CHA University, Seongnam, Korea. bjlover@lycos.co.kr
Abstract
- PURPOSE
The purpose of this study is to investigate the clinical manifestations and antibiotic resistance of salmonellosis in children.
METHODS
We reviewed medical records and investigated the clinical characteristics of culture-proven childhood salmonellosis from January 2000 through December 2011 at the CHA Bundang Medical center.
RESULTS
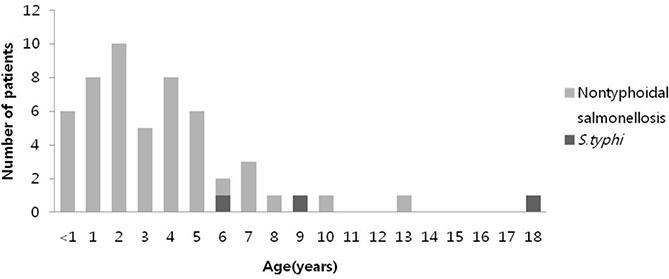
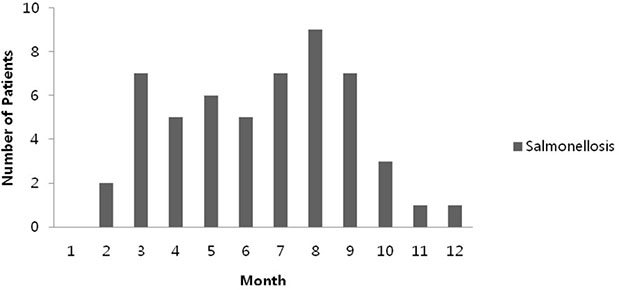
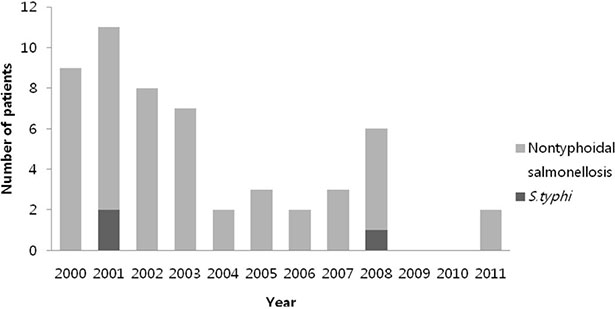
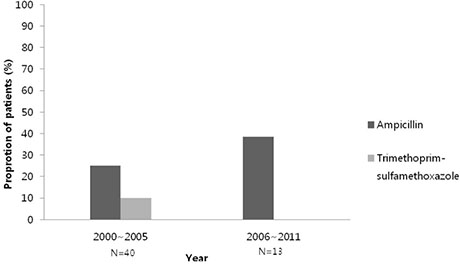
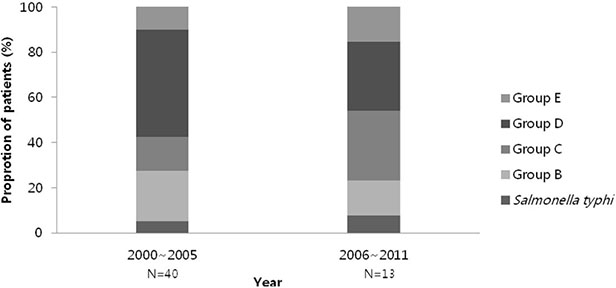
We assessed 53 patients. The median age was 3-years-old (minimum 12 days, maximum 18-years-old) and the number of male patients was 33 (62.3%). It occurred most frequently in the summer (39%) and in 2001 (11 cases) however there was no case in 2009 and 2010. Salmonella typhi was isolated in 3 cases with septicemia. Antibiotic resistance to ampicillin was most frequently presented (30.2%) and 63.6% in serogroup B. No antibiotics resistance strains were cultured in patients with positive Salmonella typhi. Admitted patients from 2000 to 2011 were divided into 2 groups; group 1 from 2000 to 2005 and group 2 from 2006 to 2011. 40 cases belonged to group 1 and 13 cases were in the group 2. Group 2 showed more resistance to ampicillin than group 1 but without any statistical significance(25% vs. 38.5%, P=0.349). In group 1, the most common serotype was group D and in group 2, the most common serotype were group C and D.
CONCLUSION
Salmonellosis in children was frequently occurred from 2000 to 2003 but decreased after 2004. There was no difference in clinical manifestations, serotypes and antibiotic resistances between the years.
Keyword
MeSH Terms
Figure
Reference
-
1. CDC. National Salmonella Surveillance Overview. 2011. Atlanta, Georgia: US Department of Health and Human Services, CDC.2. Park HM, Lee DY. Prevalence and characteristics of Salmonella spp. in Korea, 2011. Public Health Wkly Rep. 2012. 5:461–466.3. Cohen JI, Bartlett JA, Corey GR. Extra-intestinal manifestations of Salmonella infections. Medicine (Baltimore). 1987. 66:349–388.
Article4. Lee MA. Usefulness of selenite F enrichment broth for the isolation of salmonella from stool. Korean J Clin Pathol. 2000. 20:184–187.5. Lee YK, Kim JH, Hur JK, Chang KY, Kang HR, Kang JH. Salmonellosis in children in Daejeon, Korea, 1994-1999. Korean J Pediatr Infect Dis. 2000. 7:211–217.
Article6. Jeon HS, Hong YJ, Lee MI, Sohn KC. Clinical studies of salmonellosis in childhood. J Korean Pediatr Soc. 1994. 37:199–204.7. Nah SY, Park JY, Lee HJ, Seo JK. Epidemiologic and clinicalfeatures of salmonellosis in children over 10 years (1986-1995). Korean J Infect Dis. 1999. 31:129–135.8. Lim HS. Contributing factors of infectious waterborne and foodborne outbreaks in Korea. J Korean Med Assoc. 2007. 50:582–591.
Article9. Qutaishat SS, Stemper ME, Spencer SK, Borchardt MA, Opitz JC, Monson TA, et al. Transmission of Salmonella enterica serotype typhimurium DT104 to infants through mother's breast milk. Pediatrics. 2003. 111:1442–1446.
Article10. Rodrigue DC, Tauxe RV, Rowe B. International increase in Samonella enteritidis : a new pandemic? Epidemiol Infect. 1990. 105:21–27.11. Mossong J, Marques P, Ragimbeau C, Huberty-Krau P, Losch S, Meyer G, et al. Outbreaks of monophasic Salmonella enterica serovar 4,[5],12:i:-in Luxembourg, 2006. Euro Surveill. 2007. 12:E11–E12.12. Kivi M, Hofhuis A, Notermans DW, Wannet WJ, Heck ME, Van De Giessen AW, et al. A beef-associated outbreak of Salmonella Typhimurium DT104 in the Netherlands with implications for national and international policy. Epidemiol Infect. 2007. 135:890–899.
Article13. Kang HS, Cho H, Park JH, Kim JY, Paik JS. A case of Salmonella meningitis. J Korean Neurol Assoc. 2004. 22:175–176.14. Agunod M, Yamaguchi N, Lopez R. Correlative study of hydrochloric acid, pepsin, and intrinsic factor secretion in newborns and infants. Am J Dig Dis. 1969. 14:400–414.
Article15. Centers for Disease Control and Prevention. Summary of notifiable disease. United States,1994. MMWR Morb Mortal Wkly Rep. 1994. 43:1–80.16. Aserkoff B, Bennett JV. Effect of antibiotic therapy in acute salmonellosis on the fecal excretion of Salmonellae. N Engl J Med. 1969. 281:636–640.
Article17. Lim HS. Changing patterns of communicable diseases in Korea. J Prev Med Public Health. 2005. 38:117–124.18. Buchwald DS, Blaser MJ. A review of human salmonellosis. II. Duration of excretion following infection with non-typhi Salmonella. Rev Infect Dis. 1984. 6:345–356.
Article19. Kim GT, Kim JC, Song HS. Stool cultures and antibiotic therapy in cases of acute diarrhea. J Korean Soc Emerg Med. 2001. 12:64–73.20. Seo S, Lee MA. The serogroup and antimicrobial resistance of Salmonella spp. Isolated from the clinical specimens during years in a tertiary university hospital. Korean J Clin Microbiol. 2004. 7:72–76.21. Vázquez V, Calderón E, Rodríquez RS. Chloramphenicol-resistant strains of Salmonella typhosa. N Eng J Med. 1972. 286:1220.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Salmonellosis in children: Analysis of 72 Salmonella-positive culture cases during the last 10 years
- Two Children with Nontyphoidal Salmonellosis Assumed by Pets
- Salmonellosis in Children in Daejeon, Korea, 1994~1999
- Neurologic Manifestations during the Course of Neuroblastoma in Children
- Clinical Manifestation of Eosinophilic Meningitis in Korean Children: A Single Institution's Experience