Clin Exp Otorhinolaryngol.
2012 Apr;5(Suppl 1):S59-S64.
What Factors Are Associated with Good Performance in Children with Cochlear Implants? From the Outcome of Various Language Development Tests, Research on Sensory and Communicative Disorders Project in Japan: Nagasaki Experience
- Affiliations
-
- 1Kanda ENT Clinic, Nagasaki Bell Hearing Center, Nagasaki, Japan. n-bell@estate.ocn.ne.jp
- 2Department of Otolaryngology Head and Neck Surgery, Nagasaki University Graduate School of Biomedical Sciences, Nagasaki, Japan.
- 3Department of Otolaryngology Head and Neck Surgery, Nagasaki University Hospital, Nagasaki, Japan.
- 4Department of Otolaryngology Head and Neck Surgery, Okayama University Postgraduate School of Medicine, Dentistry, and Pharmaceutical Science, Okayama, Japan.
- 5The Association for Technical Aids, Tokyo, Japan.
Abstract
OBJECTIVES
We conducted multi-directional language development tests as a part of the Research on Sensory and Communicative Disorders (RSVD) in Japan. This report discusses findings as well as factors that led to better results in children with severe-profound hearing loss.
METHODS
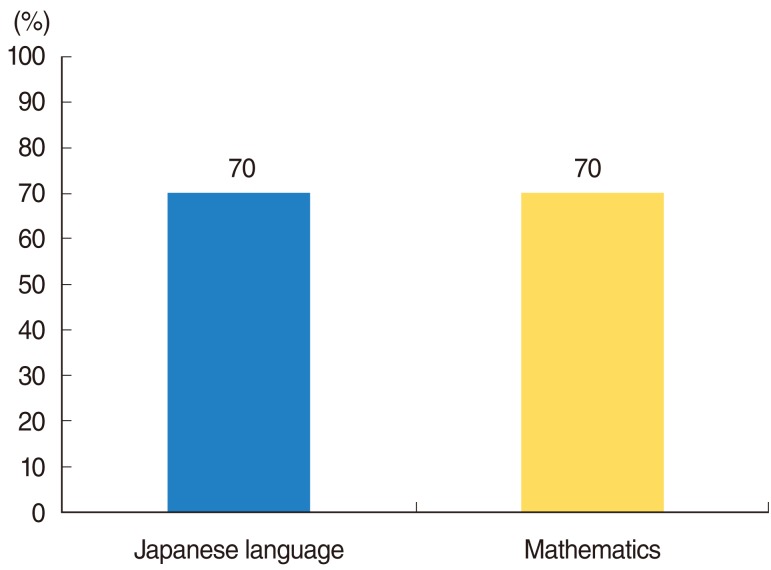
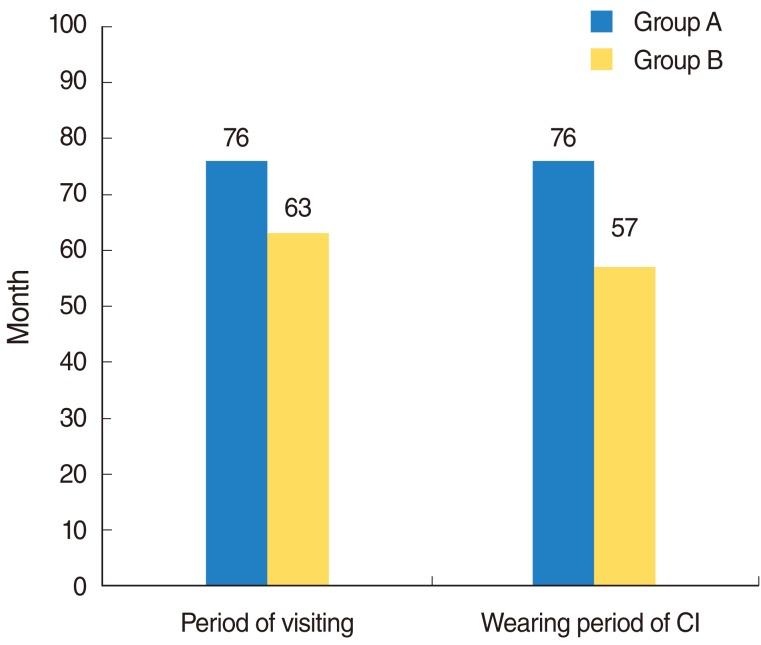
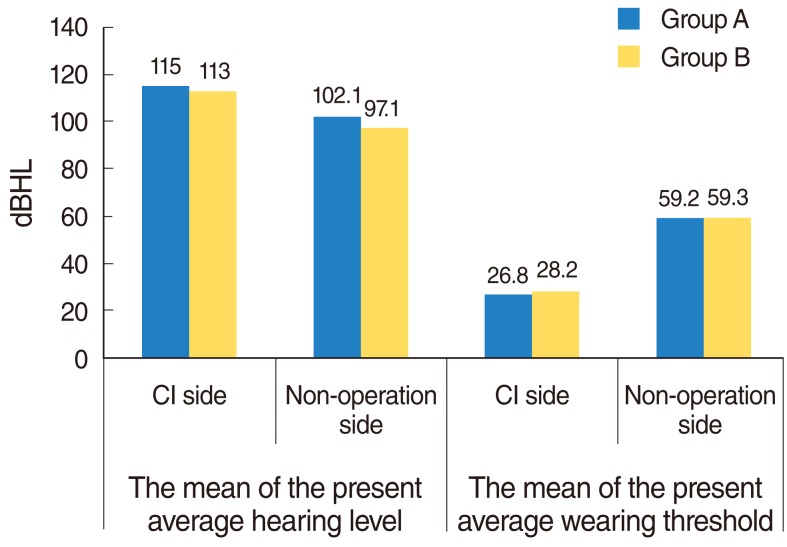
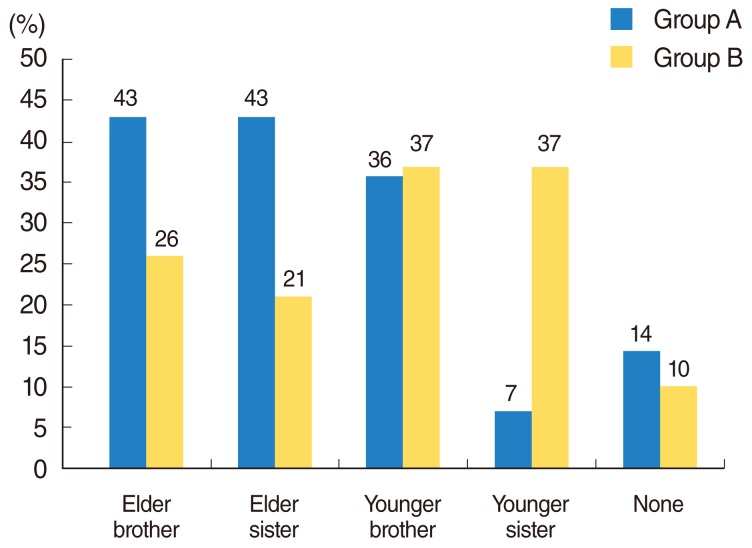
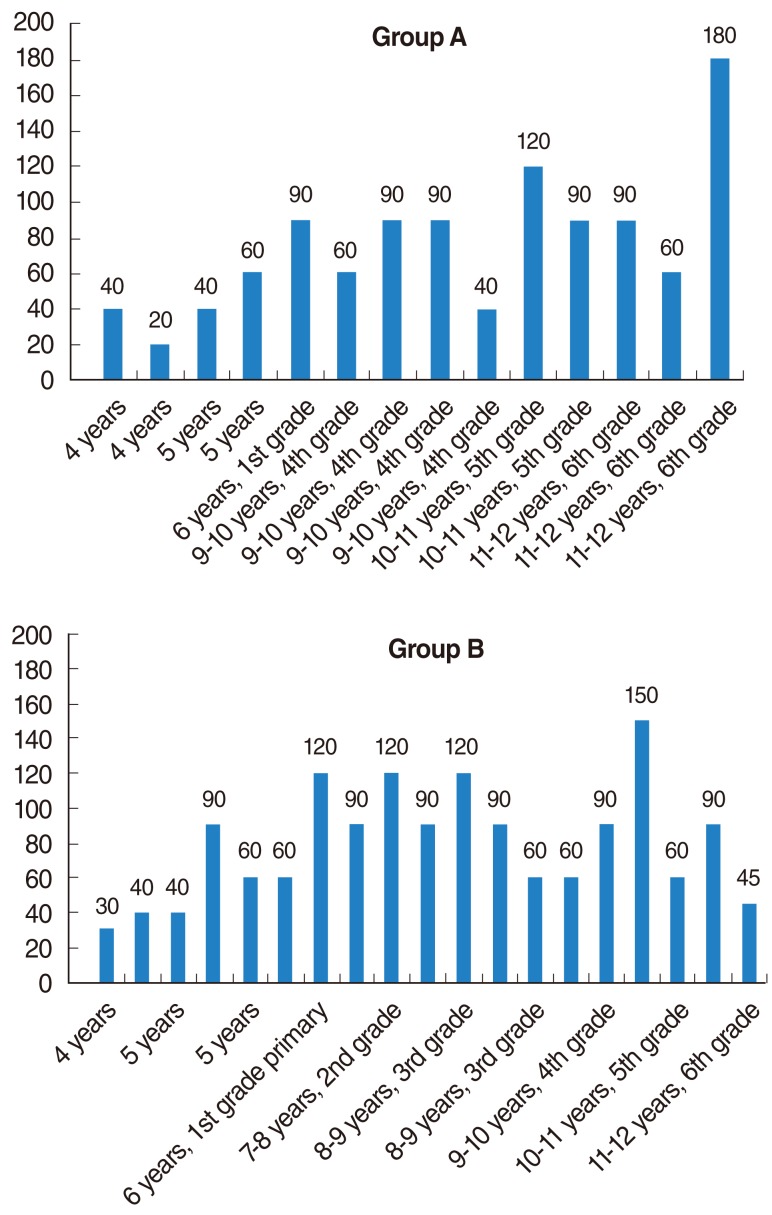
We evaluated multiple language development tests in 33 Japanese children with cochlear implants (32 patients) and hearing aid (1 patient), including 1) Test for question and answer interaction development, 2) Word fluency test, 3) Japanese version of the Peabody picture vocabulary test-revised, 4) The standardized comprehension test of abstract words, 5) The screening test of reading and writing for Japanese primary school children, 6) The syntactic processing test of aphasia, 7) Criterion-referenced testing (CRT) for Japanese language and mathematics, 8) Pervasive development disorders ASJ rating scales, and 9) Raven's colored progressive matrices. Furthermore, we investigated the factors believed to account for the better performances in these tests. The first group, group A, consisted of 14 children with higher scores in all tests than the national average for children with hearing difficulty. The second group, group B, included 19 children that scored below the national average in any of the tests.
RESULTS
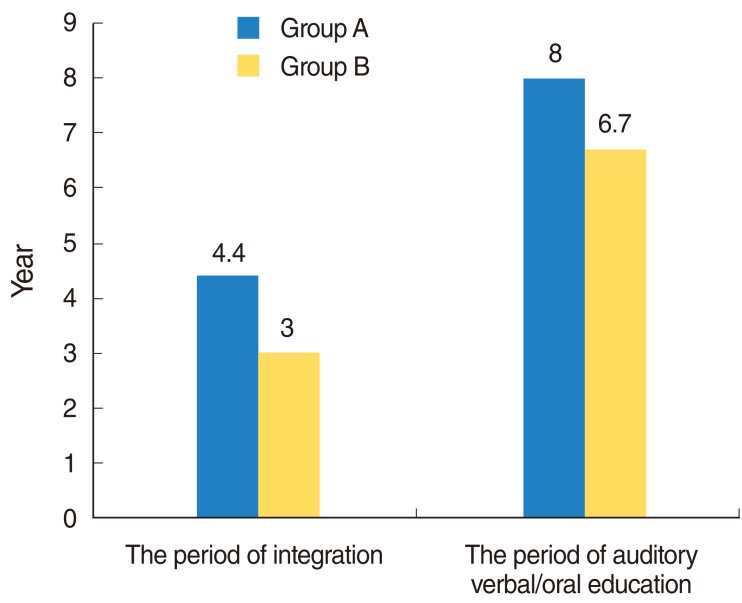
Overall, the results show that 76.2% of the scores obtained by the children in these tests exceeded the national average scores of children with hearing difficulty. The children who finished above average on all tests had undergone a longer period of regular habilitation in our rehabilitation center, had their implants earlier in life, were exposed to more auditory verbal/oral communication in their education at affiliated institutions, and were more likely to have been integrated in a regular kindergarten before moving on to elementary school.
CONCLUSION
In this study, we suggest that taking the above four factors into consideration will have an affect on the language development of children with severe-profound hearing loss.
Keyword
MeSH Terms
Figure
Reference
-
1. Meinzen-Derr J, Wiley S, Choo DI. Impact of early intervention on expressive and receptive language development among young children with permanent hearing loss. Am Ann Deaf. 2011; Winter. 155(5):580–591. PMID: 21449255.
Article2. Moon IJ, Kim EY, Chu H, Chung WH, Cho YS, Hong SH. A new measurement tool for speech development based on Ling's stages of speech acquisition in pediatric cochlear implant recipients. Int J Pediatr Otorhinolaryngol. 2011; 4. 75(4):495–499. PMID: 21295354.
Article3. Lin HC, Yang CC, Chiang YW, Hung PW, Yang EY, Wang L, et al. Effect of identification and intervention age on language development for Mandarin-speaking deaf children with high family involvement. Int J Pediatr Otorhinolaryngol. 2011; 3. 75(3):409–414. PMID: 21237520.
Article4. Wie OB. Language development in children after receiving bilateral cochlear implants between 5 and 18 months. Int J Pediatr Otorhinolaryngol. 2010; 11. 74(11):1258–1266. PMID: 20800293.
Article5. Wake M, Hughes EK, Poulakis Z, Collins C, Rickards FW. Outcomes of children with mild-profound congenital hearing loss at 7 to 8 years: a population study. Ear Hear. 2004; 2. 25(1):1–8. PMID: 14770013.
Article6. Hawker K, Ramirez-Inscoe J, Bishop DV, Twomey T, O'Donoghue GM, Moore DR. Disproportionate language impairment in children using cochlear implants. Ear Hear. 2008; 6. 29(3):467–471. PMID: 18453886.
Article7. Nikolopoulos TP, Archbold SM, Gregory S. Young deaf children with hearing aids or cochlear implants: early assessment package for monitoring progress. Int J Pediatr Otorhinolaryngol. 2005; 2. 69(2):175–186. PMID: 15656950.
Article8. Lin FR, Ceh K, Bervinchak D, Riley A, Miech R, Niparko JK. Development of a communicative performance scale for pediatric cochlear implantation. Ear Hear. 2007; 9. 28(5):703–712. PMID: 17804984.
Article9. Lin HW, Furman AC, Kujawa SG, Liberman MC. Primary neural degeneration in the Guinea pig cochlea after reversible noise-induced threshold shift. J Assoc Res Otolaryngol. 2011; 10. 12(5):605–616. PMID: 21688060.
Article10. Kral A, O'Donoghue GM. Profound deafness in childhood. N Engl J Med. 2010; 10. 07. 363(15):1438–1450. PMID: 20925546.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Language Development in Profoundly Prelingually Deaf Children with Cochlear Implantation: Long-Term Outcomes
- Language Intervention Instead of Speech Intervention for Children With Cochlear Implants
- Long Term Outcomes of Early Cochlear Implantation in Korea
- Peer Relations in Children with Cochlear Implants
- Evaluation of Speech Perception Abilities in Children with Cochlear Implants