Clin Exp Otorhinolaryngol.
2014 Jun;7(2):79-86.
Changing Patterns of Bacterial Strains in Adults and Children With Otitis Media in Korean Tertiary Care Centers
- Affiliations
-
- 1Department of Otorhinolaryngology, Kyung Hee University School of Medicine, Seoul, Korea. yeo2park@gmail.com
- 2Department of Otorhinolaryngology Head and Neck Surgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University College of Medicine, Hwaseong, Korea.
Abstract
OBJECTIVES
Otitis media (OM) is an infectious disease that affects all age brackets. Aural discharge is a typical symptom, occurring in all subtypes of OM. We have compared the identity and antibiotic sensitivity of bacteria isolated from aural discharges of adults and children with various types of OM, including acute OM (AOM), OM with effusion (OME), chronic OM (COM), and cholesteatomatous OM (CSOM).
METHODS
The study involved 2,833 patients who visited five tertiary hospitals between January 2001 and December 2010 and were diagnosed with AOM, OME, COM, or CSOM. The patients were divided into a pediatric group and an adult group, and the distribution of cultured bacteria and their antibiotic sensitivity were compared in the two groups.
RESULTS
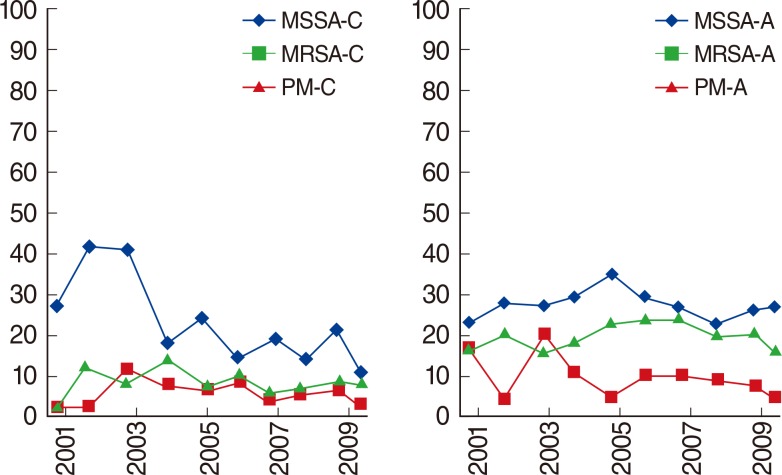
Bacterial detection rates were higher in adults than in children with OME and COM (P=0.000 each). The majority of the bacteria cultured from patients with AOM and OME bacteria were methicillin-susceptible Staphylococcus aureus (MSSA) and Streptococcus pneumoniae. Bacteria cultured from children were more susceptible to antibiotics (P=0.002) and had higher antibiotic sensitivity (P=0.001) than were bacteria cultured from adults. The majority of bacteria culture from patients with COM and CSOM were MSSA and pathogenic Pseudomonas aeruginosa. The frequency of methicillin-resistant Staphylococcus aureus was significantly higher in adults than in children, and more strains of bacteria isolated from adults were sensitive to the antibiotics septrin, vancomycin, and teicoplanin.
CONCLUSION
Bacteria cultured from children were more susceptible to antibiotics and had higher antibiotic sensitivity than did bacteria cultured from adults.
Keyword
MeSH Terms
-
Adult*
Anti-Bacterial Agents
Bacteria
Bacteriology
Child*
Communicable Diseases
Humans
Methicillin-Resistant Staphylococcus aureus
Otitis Media*
Pseudomonas aeruginosa
Staphylococcus aureus
Streptococcus pneumoniae
Teicoplanin
Tertiary Care Centers*
Vancomycin
Trimethoprim, Sulfamethoxazole Drug Combination
Anti-Bacterial Agents
Teicoplanin
Vancomycin
Figure
Reference
-
1. Alsarraf R, Jung CJ, Perkins J, Crowley C, Alsarraf NW, Gates GA. Measuring the indirect and direct costs of acute otitis media. Arch Otolaryngol Head Neck Surg. 1999; 1. 125(1):12–18. PMID: 9932581.
Article2. Gates GA. Cost-effectiveness considerations in otitis media treatment. Otolaryngol Head Neck Surg. 1996; 4. 114(4):525–530. PMID: 8643261.
Article3. Bondy J, Berman S, Glazner J, Lezotte D. Direct expenditures related to otitis media diagnoses: extrapolations from a pediatric medicaid cohort. Pediatrics. 2000; 6. 105(6):E72. PMID: 10835085.
Article4. De Neeling AJ, Van Leeuwen WJ, Van Klingeren B. Epidemiology of resistance of Streptococcus pneumonia in The Netherlands. In : The 36th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1996 Sep 15-18; New Orleans, LA.5. Therapy for children with invasive pneumococcal infections. American Academy of Pediatrics Committee on Infectious Diseases. Pediatrics. 1997; 2. 99(2):289–299. PMID: 9024464.6. Hwang JH, Chu CK, Liu TC. Changes in bacteriology of discharging ears. J Laryngol Otol. 2002; 9. 116(9):686–689. PMID: 12437801.
Article7. Yeo SG, Park DC, Hong SM, Cha CI, Kim MG. Bacteriology of chronic suppurative otitis media: a multicenter study. Acta Otolaryngol. 2007; 10. 127(10):1062–1067. PMID: 17851935.8. Jung H, Lee SK, Cha SH, Byun JY, Park MS, Yeo SG. Current bacteriology of chronic otitis media with effusion: high rate of nosocomial infection and decreased antibiotic sensitivity. J Infect. 2009; 11. 59(5):308–316. PMID: 19715725.
Article9. Rosenfeld RG. Evaluation of growth and maturation in adolescence. Pediatr Rev. 1982; 12. 4(6):175–183.
Article10. Kim CS, Jung HW, Yoo KY. Prevalence and risk factors of chronic otitis media in Korea: results of a nation-wide survey. Acta Otolaryngol. 1993; 5. 113(3):369–375. PMID: 8517141.
Article11. Kenna MA. Otitis media with effusion. In : Bailey BJ, Calhoun KH, Kohut RI, editors. Otolaryngology, head and neck surgery. 2nd ed. Philadelphia, PA: Lippincott-Raven;1998. p. 1997–2008.12. Chon KM, Yoon BN, Park SH, Lee IW, Goh EK, Wang SG, et al. Microbiologic study of the ear canal in Koreans. Korean J Otolaryngol-Head Neck Surg. 2005; 1. 48(1):8–12.13. Lee SK, Lee MS, Jung SY, Byun JY, Park MS, Yeo SG. Antimicrobial resistance of Pseudomonas aeruginosa from otorrhea of chronic suppurative otitis media patients. Otolaryngol Head Neck Surg. 2010; 10. 143(4):500–505. PMID: 20869558.
Article14. Yu YI, Cha CI, Lee IY, Byun JY, Cho JS. Current bacteriology of chonic suppurative otitis media. Korean J Otolaryngol-Head Neck Surg. 2004; 7. 47(7):607–611.15. Palva T, Karma P, Makinen J. The invasion theory. In : Sade J, editor. Cholesteatoma and mastoid surgery. Amsterdam: Kugler;1982. p. 249–264.16. Portman M. The invagination theory for the pathogenesis of cholesteatoma. In : Sade J, editor. Cholesteatoma and mastoid surgery. Amsterdam: Kugler;1982. p. 265–266.17. American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004; 5. 113(5):1451–1465. PMID: 15121972.18. Park SK. Bacteriologic study of chronic suppurative otitis media. Korean J Otolaryngol-Head Neck Surg. 1979; 3. 22(1):1–10.19. Yang HS, Kim JR, Hyun KS, Yang HC, Kim H. Bacteriologic study of chronic suppurative otitis media. Korean J Otolaryngol-Head Neck Surg. 1987; 6. 30(3):422–428.20. Ha JW, Kim YG, Kwoon SY, Choi KS, Kim CA. Bacteriologic study of chronic suppurative otitis media. Korean J Otolaryngol-Head and Neck Surg. 1995; 10. 38(10):1516–1524.21. Sim JH, Kim KT, Lee SH, Yun SH. Bacteriologic study of chronic suppurative otitis media. Korean J Otolaryngol-Head Neck Surg. 1997; 6. 40(6):819–826.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management for the Children with Otitis Media with Effusion in the Tertiary Hospital
- Management of Otitis Media in Children
- Otitis Media Following General Anesthesia: A Case Report
- Postauricular Subperiosteal and Bezold's Abscesses Complicating Chronic Suppurative Otitis Media with Cholesteatoma
- The diagnosis and management of otitis media in children