Korean J Obstet Gynecol.
2012 Dec;55(12):1020-1025. 10.5468/KJOG.2012.55.12.1020.
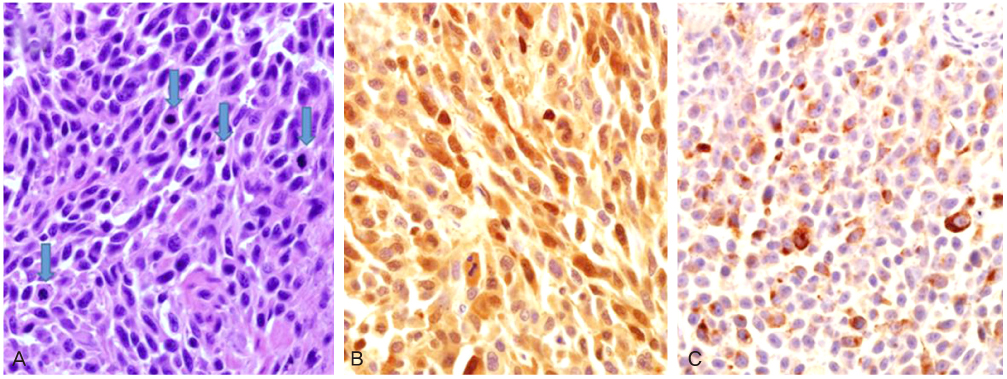
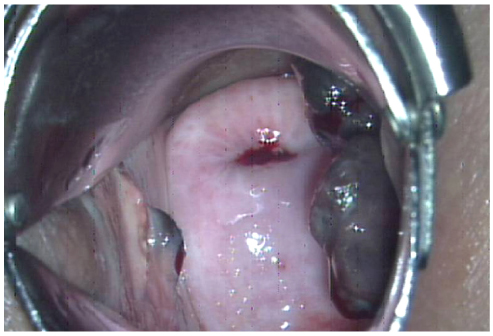
Two cases of primary malignant melanoma of vagina
- Affiliations
-
- 1Department of Obstetrics and Gynecology, The Catholic University of Korea College of Medicine, Seoul, Korea. Hursy@catholic.ac.kr
- 2Department of Obstetrics and Gynecology, Hallym University College of Medicine, Seoul, Korea.
- KMID: 2274218
- DOI: http://doi.org/10.5468/KJOG.2012.55.12.1020
Abstract
- Primary malignant melanoma of the vagina is extremly rare disease. This disease is one of non-cutaneous melanomas and accounts for 0.3% of all malignant melanomas. The most common symptoms is vaginal bleeding because the disease is usually in advanced stage at first visit. An appropriate and effective treatment protocol has not been established. The prognosis is poorer than those of other vulvar melanomas. It has been known the tumor size is the most important prognostic factor determining the survival outcome. We reported two cases of primary malignant melanoma of the vagina with review of literature.
MeSH Terms
Figure
Reference
-
1. Piura B. Management of primary melanoma of the female urogenital tract. Lancet Oncol. 2008. 9:973–981.2. Nigogosyan G, Delapava S, Pickren JW. Melanoblasts in Vaginal Mucosa. Origin for Primary Malignant Melanoma. Cancer. 1964. 17:912–913.3. Creasman WT, Phillips JL, Menck HR. The National Cancer Data Base report on cancer of the vagina. Cancer. 1998. 83:1033–1040.4. Ragnarsson-Olding B, Johansson H, Rutqvist LE, Ringborg U. Malignant melanoma of the vulva and vagina. Trends in incidence, age distribution, and long-term survival among 245 consecutive cases in Sweden 1960-1984. Cancer. 1993. 71:1893–1897.5. Ikegaya H, Iwasaki T, Matsuda I, Satodate R, Sasou S. Primary amelanotic malignant melanoma of the vagina: a case report. Gan No Rinsho. 1987. 33:1515–1523.6. Piura B, Rabinovich A, Yanai-Inbar I. Primary malignant melanoma of the vagina: case report and review of literature. Eur J Gynaecol Oncol. 2002. 23:195–198.7. Gökaslan H, Sişmanoğlu A, Pekin T, Kaya H, Ceyhan N. Primary malignant melanoma of the vagina: a case report and review of the current treatment options. Eur J Obstet Gynecol Reprod Biol. 2005. 121:243–248.8. Chung AF, Casey MJ, Flannery JT, Woodruff JM, Lewis JL Jr. Malignant melanoma of the vagina: report of 19 cases. Obstet Gynecol. 1980. 55:720–727.9. Takehara M, Ito E, Saito T, Nishioka Y, Ashihara K, Yamashita S, et al. HMB-45 staining for cytology of primary melanoma of the vagina. A case report. Acta Cytol. 2000. 44:1077–1080.10. Buchanan DJ, Schlaerth J, Kurosaki T. Primary vaginal melanoma: thirteen-year disease-free survival after wide local excision and review of recent literature. Am J Obstet Gynecol. 1998. 178:1177–1184.11. Reid GC, Schmidt RW, Roberts JA, Hopkins MP, Barrett RJ, Morley GW. Primary melanoma of the vagina: a clinicopathologic analysis. Obstet Gynecol. 1989. 74:190–199.12. Van Nostrand KM, Lucci JA 3rd, Schell M, Berman ML, Manetta A, DiSaia PJ. Primary vaginal melanoma: improved survival with radical pelvic surgery. Gynecol Oncol. 1994. 55:234–237.13. Irvin WP Jr, Bliss SA, Rice LW, Taylor PT Jr, Andersen WA. Malignant melanoma of the vagina and locoregional control: radical surgery revisited. Gynecol Oncol. 1998. 71:476–480.14. Petru E, Nagele F, Czerwenka K, Graf AH, Lax S, Bauer M, et al. Primary malignant melanoma of the vagina: long-term remission following radiation therapy. Gynecol Oncol. 1998. 70:23–26.15. Kirkwood JM, Strawderman MH, Ernstoff MS, Smith TJ, Borden EC, Blum RH. Interferon alfa-2b adjuvant therapy of high-risk resected cutaneous melanoma: the Eastern Cooperative Oncology Group Trial EST 1684. J Clin Oncol. 1996. 14:7–17.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Malignant Melanoma of the Vagina: Trial of a Wide Local Excision of Vagina and Rectum
- A Case of Primary Malignant Melanoma of the Vagina
- Malignant melanoma of the vagina: CT and MR findings
- A case of primary amelanotic melanoma of the vagina
- Cytologic Features of Papnicolaou Smears of Malignant Melanoma Arising in Vagina: A Cese Report