Korean J Obstet Gynecol.
2011 Nov;54(11):701-706. 10.5468/KJOG.2011.54.11.701.
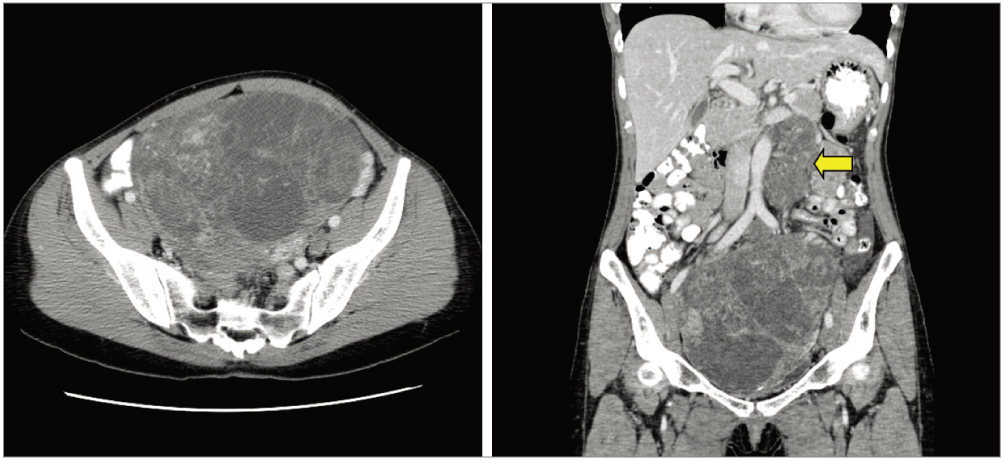
A case of complete androgen insensitivity syndrome with malignant mixed germ cell tumors
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. hyeokkim@amc.seoul.kr
- 2Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2274110
- DOI: http://doi.org/10.5468/KJOG.2011.54.11.701
Abstract
- Androgen insensitivity syndrome cases have an increased risk of developing testicular cancer due to many factors such as mutations, hormonal disturbances involving gonadotropins and cryptorchidism. However, malignant germ cell tumor is relatively rarely found compared to those seen in other types of intersex. Recently, the authors experienced a case of malignant mixed germ cell tumor with lymph node metastasis and chemotherapy resistance which was developed in a 31-year-old patient with complete androgen insensitivity syndrome.
MeSH Terms
Figure
Reference
-
1. Morris JM, Mahesh VB. Further observations on the syndrome, "Testicular Feminization". Am J Obstet Gynecol. 1963. 87:731–748.2. Manuel M, Katayama PK, Jones HW Jr. The age of occurrence of gonadal tumors in intersex patients with a Y chromosome. Am J Obstet Gynecol. 1976. 124:293–300.3. Speroff L, Fritz MA. Clinical gynecologic endocrinology and infertility. 2005. 7th ed. Philadelphia (PA): Lippincott, Williams & Williams.4. Wilkins L. Heterosexual development. The diagnosis and treatment of endocrine disorders in childhood and adolescence. 1950. Springfield (IL): Charles C Thomas;256–279.5. Hughes IA, Deeb A. Androgen resistance. Best Pract Res Clin Endocrinol Metab. 2006. 20:577–598.6. White PC, Speiser PW. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Endocr Rev. 2000. 21:245–291.7. Balducci R, Ghirri P, Brown TR, Bradford S, Boldrini A, Boscherini B, et al. A clinician looks at androgen resistance. Steroids. 1996. 61:205–211.8. Lubahn DB, Joseph DR, Sullivan PM, Willard HF, French FS, Wilson EM. Cloning of human androgen receptor complementary DNA and localization to the X chromosome. Science. 1988. 240:327–330.9. Brinkmann AO, Faber PW, van Rooij HC, Kuiper GG, Ris C, Klaassen P, et al. The human androgen receptor: domain structure, genomic organization and regulation of expression. J Steroid Biochem. 1989. 34:307–310.10. Gans SL, Rubin CL. Apparent female infants with hernias and testes. Am J Dis Child. 1962. 104:82–86.11. Gottlieb B, Pinsky L, Beitel LK, Trifiro M. Androgen insensitivity. Am J Med Genet. 1999. 89:210–217.12. Müller J, Skakkebaek NE. Testicular carcinoma in situ in children with the androgen insensitivity (testicular feminisation) syndrome. Br Med J (Clin Res Ed). 1984. 288:1419–1420.13. Chantilis SJ, McQuitty DA, Preminger GM, Marshburn PB. Laparoscopic removal of gonads containing on occult seminoma in a woman with complete androgen resistance. J Am Assoc Gynecol Laparosc. 1994. 1:277–282.14. Shahidi H, Robia M. Bilateral germ cell tumors and androgen insensitivity syndrome. J Clin Oncol. 2007. 25:4686–4688.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Laparoscopic Gonadectomy in Complete Androgen Insensitivity Syndrome
- A Case Report of Complete Androgen Insensitivity Syndrome
- A Case of Complete Androgen Insensitivity Syndrome with Bilateral Inguinal Gonads
- A case report of sisters with complete androgen insensitivity syndrome
- Mixed Germ Cell Tumor in a Patient with Turner Syndrome