Ann Rehabil Med.
2011 Dec;35(6):860-866. 10.5535/arm.2011.35.6.860.
Predictive Value of Test of Infant Motor Performance for Infants based on Correlation between TIMP and Bayley Scales of Infant Development
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Soonchunhyang University School of Medicine, Cheonan 330-721, Korea. sooapmr@schca.ac.kr
- 2Department of Occupational Medicine, Soonchunhyang University School of Medicine, Cheonan 330-721, Korea.
- KMID: 2266812
- DOI: http://doi.org/10.5535/arm.2011.35.6.860
Abstract
OBJECTIVE
To assess the relationship of scores on the test of infant motor performance (TIMP), with those on the Bayley scales of infant development (BSID), and to investigate the sensitivity and specificity of TIMP and the optimal cut-off value of TIMP scores using ROC analysis. METHOD: Seventy-six preterm and term infants were recruited from neonatal intensive care units. Subjects were tested with the TIMP at their initial visit and after 6 months, they were tested by using BSID.
RESULTS
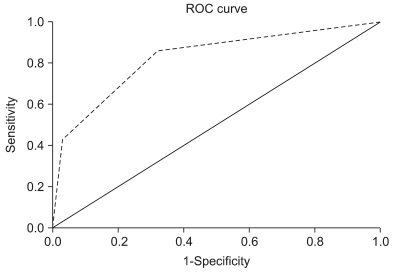
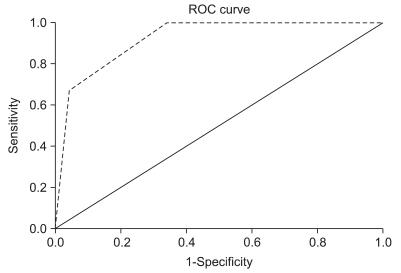
In the reliability study, TIMP scores showed highly significant correlation with the Bayley physical developmental index (BPDI) (p=0.001) and Bayley mental developmental index (BMDI) (p=0.017). Receiver operator characteristics (ROC) curve analysis was performed to evaluate the TIMP test for screening infant motor development. ROC analysis showed an area under the curve (AUC) of 0.825 (p=0.005) in BPDI and 0.992 (p=0.014) in BMDI, indicating an excellent classification performance of the model. The optimal cut-off value where a sensitivity of 86%, and specificity of 68% were achieved with the TIMP was 1.50 (between average and below average) in BPDI and where a sensitivity of 100%, and specificity of 66% were achieved with the TIMP was 1.50 in BMDI.
CONCLUSION
Our results indicate that the TIMP provides a reliable and valid measurement that can be used for the evaluation of motor function in preterm and term infants. TIMP was highly sensitive and specific with the follow-up examination of BSID. Therefore it can be used as a reliable screening tool for neonates and infants aged <4 months.
MeSH Terms
Figure
Reference
-
1. Campbell SK, Osten ET, Kolobe THA, Fisher AG. Development of the test of infant motor performance. Phys Med Rehab Clinics. 1993; 4:541–550.
Article2. Campbell SK, Kolobe THA, Osten ET, Lenke M, Girolami GL. Construct validity of the test of infant motor performance. Phys Ther. 1995; 75:585–596. PMID: 7604077.
Article3. Kim SA, Lee YJ. The test of infant motor performance (TIMP) in preterm and term infants. J Korean Acad Rehabil Med. 2010; 34:436–441.4. Edwards SL, Sarwark JF. Infant and child motor development. Clin Orthop Relat Res. 2005; 434:33–39. PMID: 15864029.
Article5. Frankenburg WK, Dodds J, Archer P, Shapiro H, Bresneck B. The Denver II: a major revision and restandardization of the Denver Developmental Screening Test. Pediatrics. 1992; 89:91–97. PMID: 1370185.
Article6. Harris SR, Megens AM, Backman CL, Hayes VE. Stability of the Bayley II Scales of Infant Development in a sample of low-risk and high-risk infants. Dev Med Child Neurol. 2005; 47:820–823. PMID: 16288672.
Article7. Bayley N. Bayley scales of infant development. 1993. 2nd ed. New York: The Psychological Corporation;p. 1–188.8. Kolobe TH, Bulanda M, Susman L. Predicting motor outcome at preschool age for infants tested at 7, 30, 60 and 90 days after term age using the Test of Infant Motor Performance. Phys Ther. 2004; 84:1144–1156. PMID: 15563255.
Article9. Piper MC, Mazer B, Silver KM, Ramsay M. Resolution of neurological symptoms in high-risk infants during the first two years of life. Dev Med Child Neurol. 1988; 30:26–35. PMID: 3371568.
Article10. Leonard CH, Clyman RI, Piecuch RE, Juster RP, Ballard RA, Behle MB. Effect of medical and social risk factors on outcome of prematurity and very low birth weight. J Pediatr. 1990; 116:620–626. PMID: 2319409.
Article11. Campbell SK, Hedeker D. Validity of the Test of Infant Motor Performance for discriminating among infants with varying risk for poor motor outcome. J Pediatr. 2001; 139:546–551. PMID: 11598602.
Article12. Rose RU, Westcott SL. Responsiveness of the Test of Infant Motor Performance (TIMP) in infants born preterm. Pediatr Phys Ther. 2005; 17:219–224. PMID: 16357676.
Article13. Campbell SK. Test-retest reliability of the test of Infant Motor Performance. Pediatr Phys Ther. 1999; 11:60–66.
Article14. Campbell SK, Kolobe TH. Concurrent validity of the test of infant motor performance with the Alberta infant motor scale. Pediatr Phys Ther. 2000; 12:2–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Test of Infant Motor Performance (TIMP) in Preterm and Term Infants
- Assessment of Preterm Infants Using the Bayley-III Scales in Korea
- Comparative Study between Bayley Scales of Infant Development-II and Korean Infant and Child Developmental Test in Infants Younger than 12 Months
- The Validity of Two Neuromotor Assessments for Predicting Motor Performance at 12 Months in Preterm Infants
- Assessment of children with developmental delay: Korean infant and child development test (KICDT) and Korean Bayley scale of infant development-II (K-BSID-II)