Ann Rehabil Med.
2013 Aug;37(4):547-555. 10.5535/arm.2013.37.4.547.
Plain Abdominal Radiograph as an Evaluation Method of Bowel Dysfunction in Patients With Spinal Cord Injury
- Affiliations
-
- 1Department of Rehabilitation Medicine, Wonkwang University School of Medicine, Iksan, Korea. mcjoo68@wku.ac.kr
- 2Institute of Wonkwang Medical Science, Wonkwang University School of Medicine, Iksan, Korea.
- 3Department of Diagnostic Radiology, Wonkwang University School of Medicine, Iksan, Korea.
- KMID: 2266611
- DOI: http://doi.org/10.5535/arm.2013.37.4.547
Abstract
OBJECTIVE
To evaluate the usefulness of plain abdominal radiography as an evaluation method for bowel dysfunction in patients with spinal cord injury (SCI).
METHODS
Forty-four patients with SCI were recruited. Patients were interviewed about their clinical symptoms, and the constipation score and Bristol stool form scale were assessed. The colon transit time (CTT) was measured by using radio-opaque markers (Kolomark). The degree of stool retention and the presence of megacolon or megarectum were evaluated using plain abdominal radiographs. We examined the relationship between clinical aspects and CTT and plain abdominal radiography.
RESULTS
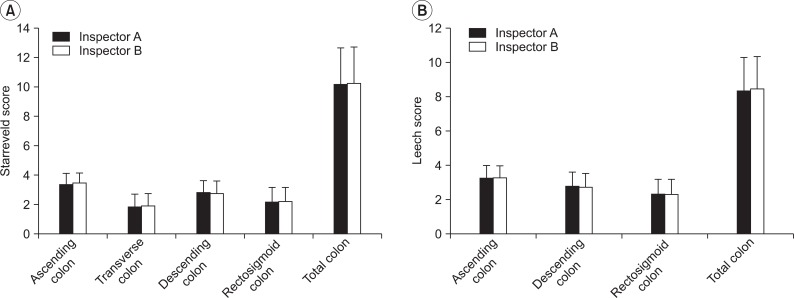
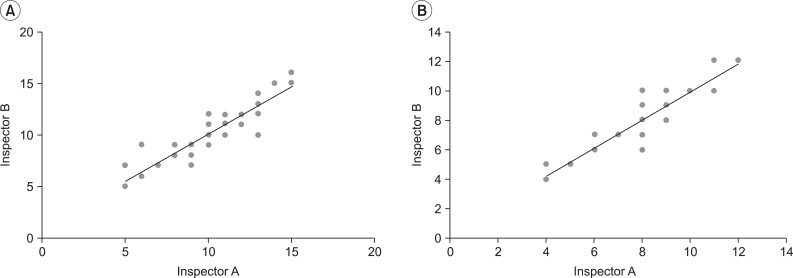
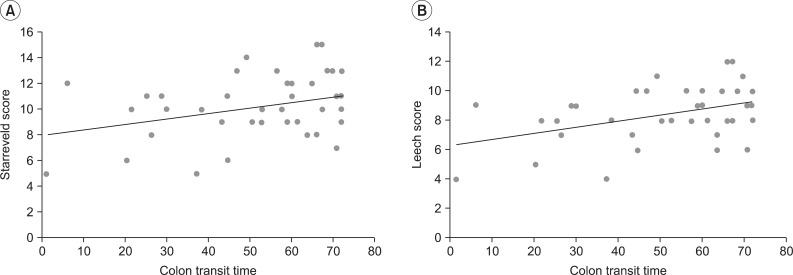
The constipation scores ranged from 1 to 13, and the average was 4.19+/-3.11, and the Bristol stool form scale ranged from 1 to 6, with an average of 4.13+/-1.45. CTTs were 19.3+/-16.17, 19.3+/-13.45, 15.32+/-13.15, and 52.42+/-19.14 in the right, left, rectosigmoid, and total colon. Starreveld scores were 3.4+/-0.7, 1.8+/-0.86, 2.83+/-0.82, 2.14+/-1, and 10.19+/-2.45 in the ascending, transverse, descending, rectosigmoid, and total colon. Leech scores were 3.28+/-0.7, 2.8+/-0.8, 2.35+/-0.85, and 8.45+/-1.83 in the right, left, rectosigmoid, and total colon. The number of patients with megacolon and megarectum was 14 (31.8%) and 11 (25%). There were statistically significant correlations between the total CTT and constipation score (p<0.05), and Starreveld and Leech scores (p<0.05). Significant correlations were observed between each segmental CTT and the segmental stool retention score (p<0.05).
CONCLUSION
Plain abdominal radiography is useful as a convenient and simple method of evaluation of bowel dysfunction in patients with SCI.
MeSH Terms
Figure
Cited by 1 articles
-
Diagnostic Value of Plain Abdominal Radiography in Stroke Patients With Bowel Dysfunction
Hyo Jeong Moon, Se Eung Noh, Ji Hee Kim, Min Cheol Joo
Ann Rehabil Med. 2015;39(2):243-252. doi: 10.5535/arm.2015.39.2.243.
Reference
-
1. Coggrave M, Norton C, Wilson-Barnett J. Management of neurogenic bowel dysfunction in the community after spinal cord injury: a postal survey in the United Kingdom. Spinal Cord. 2009; 47:323–330. PMID: 19015665.
Article2. Seo JH, Song KS, Ko MH, Park SH. The change of neurogenic bowel dysfunction in spinal cord injury patients during admission. J Korean Acad Rehabil Med. 2009; 33:441–447.3. Ashraf W, Park F, Lof J, Quigley EM. An examination of the reliability of reported stool frequency in the diagnosis of idiopathic constipation. Am J Gastroenterol. 1996; 91:26–32. PMID: 8561138.4. Starreveld JS, Pols MA, Van Wijk HJ, Bogaard JW, Poen H, Smout AJ. The plain abdominal radiograph in the assessment of constipation. Z Gastroenterol. 1990; 28:335–338. PMID: 2238762.5. Halligan S, Bartram CI. The radiological investigation of constipation. Clin Radiol. 1995; 50:429–435. PMID: 7614787.
Article6. Leech SC, McHugh K, Sullivan PB. Evaluation of a method of assessing faecal loading on plain abdominal radiographs in children. Pediatr Radiol. 1999; 29:255–258. PMID: 10199902.
Article7. Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999; 45(Suppl 2):II43–II47. PMID: 10457044.
Article8. Heaton KW, Radvan J, Cripps H, Mountford RA, Braddon FE, Hughes AO. Defecation frequency and timing, and stool form in the general population: a prospective study. Gut. 1992; 33:818–824. PMID: 1624166.
Article9. Arhan P, Devroede G, Jehannin B, Lanza M, Faverdin C, Dornic C, et al. Segmental colonic transit time. Dis Colon Rectum. 1981; 24:625–629. PMID: 7318630.
Article10. Margulis AR, Burhenne HJ. Practical alimentary tract radiology. Boston: Mosby Year Book;1993.11. Glickman S, Kamm MA. Bowel dysfunction in spinal-cord-injury patients. Lancet. 1996; 347:1651–1653. PMID: 8642958.
Article12. Ng C, Prott G, Rutkowski S, Li Y, Hansen R, Kellow J, et al. Gastrointestinal symptoms in spinal cord injury: relationships with level of injury and psychologic factors. Dis Colon Rectum. 2005; 48:1562–1568. PMID: 15981066.
Article13. De Looze DA, De Muynck MC, Van Laere M, De Vos MM, Elewaut AG. Pelvic floor function in patients with clinically complete spinal cord injury and its relation to constipation. Dis Colon Rectum. 1998; 41:778–786. PMID: 9645749.
Article14. Keshavarzian A, Barnes WE, Bruninga K, Nemchausky B, Mermall H, Bushnell D. Delayed colonic transit in spinal cord-injured patients measured by indium-111 Amberlite scintigraphy. Am J Gastroenterol. 1995; 90:1295–1300. PMID: 7639233.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neurogenic Bowel Dysfunction in Spinal Cord Injury Patients
- The Change of Neurogenic Bowel Dysfunction in Spinal Cord Injury Patients during Admission
- Rehabilitation of neurogenic bladder and bowel after spinal cord injury
- Intracavernous Papaverine Injection for Erectile Impotence in Men with Spinal Cord Injury
- Chronic Gastrointestinal Problems and Bowel Dysfunction in Spinal Cord Injury Patients