Ann Rehabil Med.
2013 Oct;37(5):725-729. 10.5535/arm.2013.37.5.725.
Thoracic Infectious Spondylitis After Surgical Treatments of Herniated Lumbar Intervertebral Disc
- Affiliations
-
- 1Department of Rehabilitation Medicine, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea. kohse@kuh.ac.kr
- KMID: 2266593
- DOI: http://doi.org/10.5535/arm.2013.37.5.725
Abstract
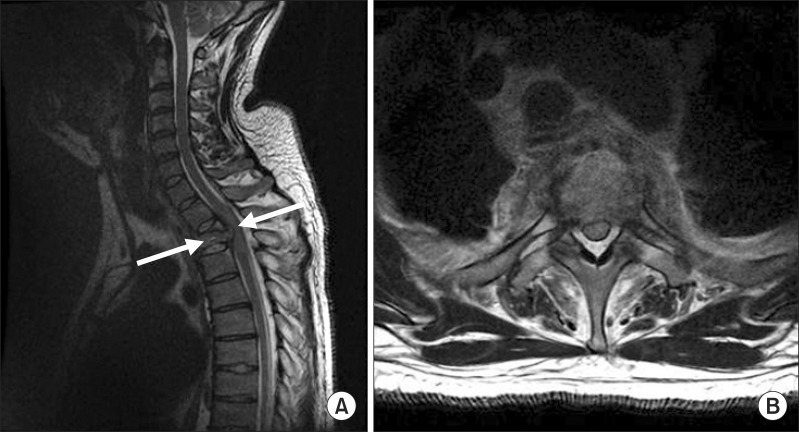
- The postoperative infectious spondylitis has been reported to occur among every 1% to 12%. It is difficult to early diagnose in some cases. If the diagnosis is delayed, it can be a life-threatening condition. We report a 32-year-old male patient with postoperative infectious spondylitis. He had surgical treatments for traumatic intervertebral disc herniations in L3-4 and L4-5. Three weeks after surgery, he complained for fever and paraplegia. Cervicothoracic magnetic resonance imaging showed the collapsed T2 and T3 vertebral body with changes of bone marrow signal intensity. Moreover, it showed anterior and posterior epidural masses causing spinal cord compressions which suggested infectious spondylitis. After the use of antibiotics and surgical decompressions T2-T3, his general conditions were improved and muscle power of lower extremities began to be gradually restored. However, we could not identify the exact organisms that may be the cause of infectious spondylitis. It could be important that the infectious spondylitis, which is presented away from the primary operative level, should be observed in patients with fevers of unknown origin and paraplegia.
MeSH Terms
Figure
Reference
-
1. An KC, Kim KY, Heo MJ, Kim JS. Monitoring for deep wound infection after thoracolumbar surgery significance of suction drainage tip culture for early detection of postoperative deep wound infection. J Korean Soc Spine Surg. 2006; 13:23–31.
Article2. Lee CS. Pyogenic infection of the spine. J Korean Soc Spine Surg. 1999; 6:247–255.3. Ha KY, Wee D, Park SJ, Yeon G, Han SG. Latent multiple noncontiguous pyogenic spondylitis: a case report. J Korean Orthop Assoc. 1997; 32:517–522.
Article4. Lohr M, Reithmeier T, Ernestus RI, Ebel H, Klug N. Spinal epidural abscess: prognostic factors and comparison of different surgical treatment strategies. Acta Neurochir (Wien). 2005; 147:159–166. PMID: 15570436.
Article5. Gerometta A, Bittan F, Rodriguez Olaverri JC. Postoperative spondilodiscitis. Int Orthop. 2012; 36:433–438. PMID: 22307558.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Spontaneous Resorption of Herniated Lumbar Disc: A case report
- Histological Composition of the Extruded Intervertebral Disc in Lumbar Intervertebral Disc Herniation
- A Clinical Study of Herniated Lumbar Intervertebral Disc in Teenagers
- Percutaneous Discectomy of Herniated Intervertebral Disc with a Dekompressor(R)
- Spinal Nerve Root Swelling Mimicking Intervertebral Disc Herniation in Magnetic Resonance Imaging: A Case Report