Ann Dermatol.
2010 Nov;22(4):373-378. 10.5021/ad.2010.22.4.373.
What Should Be Considered in Treatment of Melasma
- Affiliations
-
- 1Department of Dermatology, Ajou University School of Medicine, Suwon, Korea.
- 2Department of Dermatology, Archet-2 Hospital, Nice, France. ortonne@unice.fr
- KMID: 2266172
- DOI: http://doi.org/10.5021/ad.2010.22.4.373
Abstract
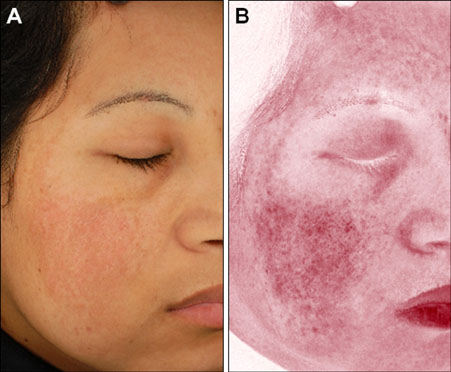
- Melasma is a common acquired hyperpigmentary skin disorder characterized by light to dark brown macules and patches occurring in the sun-exposed areas of the face. Melasma lesional skin is characterized by epidermal hyperpigmentation through increased melanogenesis in epidermal melanocytes. Some patients have dermal melanin but its amount is not significant and its distribution is very heterogeneous in the whole melasma lesional skin. Melasma is not homogeneous disease and there are personal characteristics of patients with melasma. The pathogenesis of melasma is not fully understood, but several hypotheses have been suggested. Increased vascularity in melasma lesions has suggested the role of increased number of enlarged vessels in the development of melasma. Endogeneous and exogeneous stimuli such as sex hormones and ultraviolet irradiation respectively may stimulate the microenvironment leading to the release of various mediators that cause activation of melanocytes and/or these stimuli may directly activate the melanocytes. Melasma patients may have specialized melanocytes with an intrinsic sensitivity to these stimuli.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Possible Involvement of Keratinocyte Growth Factor in the Persistence of Hyperpigmentation in both Human Facial Solar Lentigines and Melasma
Kiyotaka Hasegawa, Rumiko Fujiwara, Kiyoshi Sato, Jaeyoung Shin, Sang Jin Kim, Misun Kim, Hee Young Kang
Ann Dermatol. 2015;27(5):626-629. doi: 10.5021/ad.2015.27.5.626.
Reference
-
1. Ortonne JP, Arellano I, Berneburg M, Cestari T, Chan H, Grimes P, et al. A global survey of the role of ultraviolet radiation and hormonal influences in the development of melasma. J Eur Acad Dermatol Venereol. 2009. 23:1254–1262.
Article2. Kang HY, Valerio L, Bahadoran P, Ortonne JP. The role of topical retinoids in the treatment of pigmentary disorders: an evidence-based review. Am J Clin Dermatol. 2009. 10:251–260.3. Ortonne JP, Passeron T. Melanin pigmentary disorders: treatment update. Dermatol Clin. 2005. 23:209–226.
Article4. Negishi K, Kushikata N, Tezuka Y, Takeuchi K, Miyamoto E, Wakamatsu S. Study of the incidence and nature of "very subtle epidermal melasma" in relation to intense pulsed light treatment. Dermatol Surg. 2004. 30:881–886.
Article5. Lee HS, Won CH, Lee DH, An JS, Chang HW, Lee JH, et al. Treatment of melasma in Asian skin using a fractional 1,550-nm laser: an open clinical study. Dermatol Surg. 2009. 35:1499–1504.6. Jeong SY, Chang SE, Bak H, Choi JH, Kim IH. New melasma treatment by collimated low fluence Q-switched Nd:YAG laser. Korean J Dermatol. 2008. 46:1163–1170.7. Polnikorn N. Treatment of refractory dermal melasma with the MedLite C6 Q-switched Nd:YAG laser: two case reports. J Cosmet Laser Ther. 2008. 10:167–173.
Article8. Cho SB, Kim JS, Kim MJ. Melasma treatment in Korean women using a 1064-nm Q-switched Nd:YAG laser with low pulse energy. Clin Exp Dermatol. 2009. 34:e847–e850.
Article9. Kim MJ, Kim JS, Cho SB. Punctate leucoderma after melasma treatment using 1064-nm Q-switched Nd:YAG laser with low pulse energy. J Eur Acad Dermatol Venereol. 2009. 23:960–962.
Article10. Sanchez NP, Pathak MA, Sato S, Fitzpatrick TB, Sanchez JL, Mihm MC Jr. Melasma: a clinical, light microscopic, ultrastructural, and immunofluorescence study. J Am Acad Dermatol. 1981. 4:698–710.
Article11. Grimes PE, Yamada N, Bhawan J. Light microscopic, immunohistochemical, and ultrastructural alterations in patients with melasma. Am J Dermatopathol. 2005. 27:96–101.
Article12. Sarvjot V, Sharma S, Mishra S, Singh A. Melasma: a clinicopathological study of 43 cases. Indian J Pathol Microbiol. 2009. 52:357–359.
Article13. Lawrence N, Cox SE, Brody HJ. Treatment of melasma with Jessner's solution versus glycolic acid: a comparison of clinical efficacy and evaluation of the predictive ability of Wood's light examination. J Am Acad Dermatol. 1997. 36:589–593.
Article14. Kang HY, Bahadoran P, Suzuki I, Zugaj D, Khemis A, Passeron T, et al. In vivo reflectance confocal microscopy detects pigmentary changes in melasma at a cellular level resolution. Exp Dermatol. 2010. 19:e228–e233.
Article15. Kang WH, Yoon KH, Lee ES, Kim J, Lee KB, Yim H, et al. Melasma: histopathological characteristics in 56 Korean patients. Br J Dermatol. 2002. 146:228–237.
Article16. Moncada B, Sahagún-Sánchez LK, Torres-Alvarez B, Castanedo-Cázares JP, Martínez-Ramírez JD, González FJ. Molecular structure and concentration of melanin in the stratum corneum of patients with melasma. Photodermatol Photoimmunol Photomed. 2009. 25:159–160.
Article17. Kim EH, Kim YC, Lee ES, Kang HY. The vascular characteristics of melasma. J Dermatol Sci. 2007. 46:111–116.
Article18. Kim EJ, Park HY, Yaar M, Gilchrest BA. Modulation of vascular endothelial growth factor receptors in melanocytes. Exp Dermatol. 2005. 14:625–633.
Article19. Jo HY, Kim CK, Suh IB, Ryu SW, Ha KS, Kwon YG, et al. Co-localization of inducible nitric oxide synthase and phosphorylated Akt in the lesional skins of patients with melasma. J Dermatol. 2009. 36:10–16.
Article20. Mahmoud BH, Ruvolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, et al. Impact of long-wavelength UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010. 130:2092–2097.
Article21. Hernández-Barrera R, Torres-Alvarez B, Castanedo-Cazares JP, Oros-Ovalle C, Moncada B. Solar elastosis and presence of mast cells as key features in the pathogenesis of melasma. Clin Exp Dermatol. 2008. 33:305–308.
Article22. Suzuki I, Kato T, Motokawa T, Tomita Y, Nakamura E, Katagiri T. Increase of pro-opiomelanocortin mRNA prior to tyrosinase, tyrosinase-related protein 1, dopachrome tautomerase, Pmel-17/gp100, and P-protein mRNA in human skin after ultraviolet B irradiation. J Invest Dermatol. 2002. 118:73–78.
Article23. Im S, Kim J, On WY, Kang WH. Increased expression of alpha-melanocyte-stimulating hormone in the lesional skin of melasma. Br J Dermatol. 2002. 146:165–167.24. Kang HY, Hwang JS, Lee JY, Ahn JH, Kim JY, Lee ES, et al. The dermal stem cell factor and c-kit are overexpressed in melasma. Br J Dermatol. 2006. 154:1094–1099.
Article25. Imokawa G. Autocrine and paracrine regulation of melanocytes in human skin and in pigmentary disorders. Pigment Cell Res. 2004. 17:96–110.
Article26. Rhodes LE, Gledhill K, Masoodi M, Haylett AK, Brownrigg M, Thody AJ, et al. The sunburn response in human skin is characterized by sequential eicosanoid profiles that may mediate its early and late phases. FASEB J. 2009. 23:3947–3956.
Article27. Kapoor R, Phiske MM, Jerajani HR. Evaluation of safety and efficacy of topical prostaglandin E2 in treatment of vitiligo. Br J Dermatol. 2009. 160:861–863.
Article28. Hexsel D, Rodrigues TC, Dal'Forno T, Zechmeister-Prado D, Lima MM. Melasma and pregnancy in southern Brazil. J Eur Acad Dermatol Venereol. 2009. 23:367–368.
Article29. Moin A, Jabery Z, Fallah N. Prevalence and awareness of melasma during pregnancy. Int J Dermatol. 2006. 45:285–288.
Article30. Pérez M, Sánchez JL, Aguiló F. Endocrinologic profile of patients with idiopathic melasma. J Invest Dermatol. 1983. 81:543–545.
Article31. Jee SH, Lee SY, Chiu HC, Chang CC, Chen TJ. Effects of estrogen and estrogen receptor in normal human melanocytes. Biochem Biophys Res Commun. 1994. 199:1407–1412.
Article32. Kippenberger S, Loitsch S, Solano F, Bernd A, Kaufmann R. Quantification of tyrosinase, TRP-1, and Trp-2 transcripts in human melanocytes by reverse transcriptase-competitive multiplex PCR--regulation by steroid hormones. J Invest Dermatol. 1998. 110:364–367.
Article33. Lieberman R, Moy L. Estrogen receptor expression in melasma: results from facial skin of affected patients. J Drugs Dermatol. 2008. 7:463–465.34. Jang YH, Lee JY, Kang HY, Lee ES, Kim YC. Oestrogen and progesterone receptor expression in melasma: an immunohistochemical analysis. J Eur Acad Dermatol Venereol. Forthcoming 2010.
Article35. Kim NH, Lee CH, Lee AY. H19 RNA downregulation stimulated melanogenesis in melasma. Pigment Cell Melanoma Res. 2010. 23:84–92.
Article