Ann Dermatol.
2014 Aug;26(4):514-516. 10.5021/ad.2014.26.4.514.
Green Nail Syndrome Treated with the Application of Tobramycin Eye Drop
- Affiliations
-
- 1Department of Dermatology, Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea.
- 2Department of Dermatology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea. ylpark@schmc.ac.kr
- 3Department of Dermatology, Soonchunhyang University Cheonan Hospital, Cheonan, Korea.
- KMID: 2265596
- DOI: http://doi.org/10.5021/ad.2014.26.4.514
Abstract
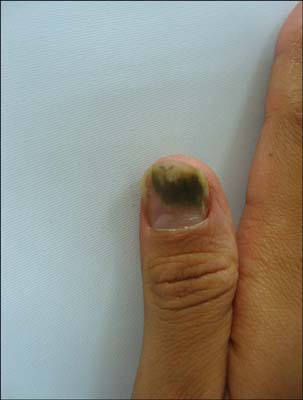
- Green nail syndrome (chromonychia) is a nail disorder characterized by onycholysis and green-black discoloration of the nail bed. This condition is often associated with chronic paronychia. Pseudomonas aeruginosa is the most commonly identified organism in cultures from the affected area. Despite the various treatment options available, removal of the nail is still necessary in many cases. A 35-year-old man presented with dark-greenish discoloration of the nail plate and onycholysis on the left thumbnail. He had been treated with oral antifungal and antibiotic agents for several months; however, the lesion showed no improvement. The diagnosis of green nail syndrome was established after a positive bacterial culture, and on the basis of the antibiotic sensitivity test result, tobramycin eye drop (Tobrex(R)) was then prescribed. Three weeks later, the nail discoloration almost vanished but the onycholysis remained. Herein, we recommend the application of tobramycin eye drop as an easy and safe treatment option for green nail syndrome.
Figure
Reference
-
1. James WD, Berger TG, Elston DM, Odom RB. Andrews' diseases of the skin: clinical dermatology. 10th ed. Philadelphia: Saunders Elsevier;2006.2. Cohen MS, Rutala WA, Weber DJ. Gram-negative coccal and bacillary infections. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: Mc-Graw-Hill;2012. p. 2183–2186.3. Greene SL, Su WP, Muller SA. Pseudomonas aeruginosa infections of the skin. Am Fam Physician. 1984; 29:193–200.4. Wu DC, Chan WW, Metelitsa AI, Fiorillo L, Lin AN. Pseudomonas skin infection: clinical features, epidemiology, and management. Am J Clin Dermatol. 2011; 12:157–169.5. Agger WA, Mardan A. Pseudomonas aeruginosa infections of intact skin. Clin Infect Dis. 1995; 20:302–308.
Article6. Rigopoulos D, Rallis E, Gregoriou S, Larios G, Belyayeva Y, Gkouvi K, et al. Treatment of pseudomonas nail infections with 0.1% octenidine dihydrochloride solution. Dermatology. 2009; 218:67–68.
Article7. Cunha BA. Pseudomonas aeruginosa: resistance and therapy. Semin Respir Infect. 2002; 17:231–239.
Article8. Murdan S. Enhancing the nail permeability of topically applied drugs. Expert Opin Drug Deliv. 2008; 5:1267–1282.
Article9. Shivakumar HN, Juluri A, Desai BG, Murthy SN. Ungual and transungual drug delivery. Drug Dev Ind Pharm. 2012; 38:901–911.
Article10. Brogden RN, Pinder RM, Sawyer PR, Speight TM, Avery GS. Tobramycin: a review of its antibacterial and pharmacokinetic properties and therapeutic use. Drugs. 1976; 12:166–200.