Allergy Asthma Immunol Res.
2010 Jan;2(1):55-58. 10.4168/aair.2010.2.1.55.
Cutaneous leukocytoclastic vasculitis due to anti-tuberculosis medications, rifampin and pyrazinamide
- Affiliations
-
- 1Department of Allergy and Rheumatology, Ajou University School of Medicine, Suwon, Korea. ye9007@ajou.ac.kr
- 2Department of Pathology, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2260420
- DOI: http://doi.org/10.4168/aair.2010.2.1.55
Abstract
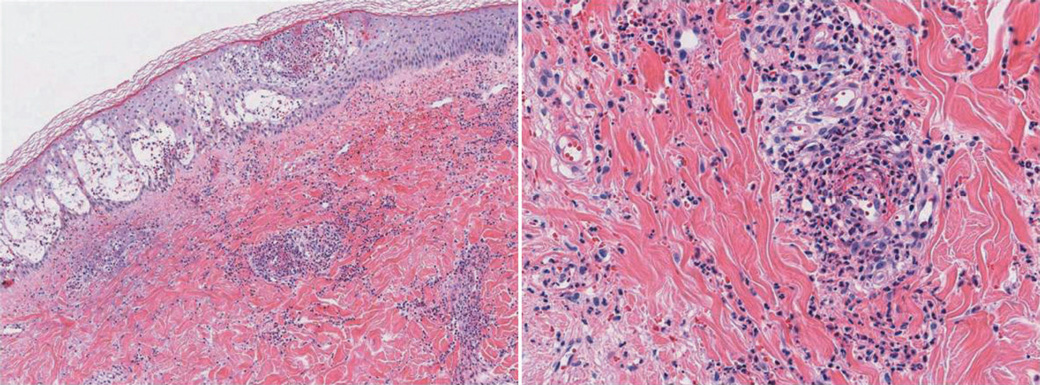
- Anti-tuberculosis drugs frequently result in cutaneous adverse reactions, including pruritus, maculopapular exanthems, and urticaria. However, anti-tuberculosis drug-associated cutaneous leukocytoclastic vasculitis (CLV) has been rarely reported. We describe a case of CLV induced by rifampin and pyrazinamide. A 38-year-old male had been diagnosed with pulmonary tuberculosis two months ago and then he started standard anti-tuberculosis therapy with isoniazid, rifampin, ethambutol, and pyrazinamide. Purpuric lesions developed in the extremities after 1.5 months of anti-tuberculosis medication; the lesions progressively spread over the entire body. Histopathology of the purpuric skin lesion was consistent with leukocytoclastic vasculitis. The skin lesion improved after cessation of anti-tuberculosis medications and treatment with oral corticosteroids and antihistamines. Anti-tuberculosis drugs were rechallenged one at a time over 3 days. Purpura recurred on the right forearm and forehead after taking 300 mg of rifampin. The skin lesion disappeared after taking oral prednisolone. Finally, 1,500 mg of pyrazinamide was readministrated, and then purpuric lesions recurred on both forearms. This report describes a case of leukocytoclastic vasculitis secondary to rifampin and pyrazinamide therapy.
MeSH Terms
-
Adrenal Cortex Hormones
Adult
Ethambutol
Exanthema
Extremities
Forearm
Forehead
Histamine Antagonists
Humans
Isoniazid
Male
Prednisolone
Pruritus
Purpura
Pyrazinamide
Rifampin
Skin
Tuberculosis, Pulmonary
Urticaria
Vasculitis
Vasculitis, Leukocytoclastic, Cutaneous
Adrenal Cortex Hormones
Ethambutol
Histamine Antagonists
Isoniazid
Prednisolone
Pyrazinamide
Rifampin
Vasculitis, Leukocytoclastic, Cutaneous
Figure
Reference
-
1. Crowson AN, Mihm MC Jr, Magro CM. Cutaneous vasculitis: a review. J Cutan Pathol. 2003. 30:161–173.2. Justiniano H, Berlingeri-Ramos AC, Sanchez JL. Pattern analysis of drug-induced skin diseases. Am J Dermatopathol. 2008. 30:352–369.3. Khasnis A, Langford CA. Update on vasculitis. J Allergy Clin Immunol. 2009. 123:1226–1236.4. Carvalho M, Dominoni RL, Senchechen D, Fernandes AF, Burigo IP, Doubrawa E. Cutaneous leukocytoclastic vasculitis accompanied by pulmonary tuberculosis. J Bras Pneumol. 2008. 34:745–748.5. Chan CH, Chong YW, Sun AJ, Hoheisel GB. Cutaneous vasculitis associated with tuberculosis and its treatment. Tubercle. 1990. 71:297–300.6. Iredale JP, Sankaran R, Wathen CG. Cutaneous vasculitis associated with rifampin therapy. Chest. 1989. 96:215–216.7. Kim HR, Park BH, Son J-Y, Jung JY, Ahn JR, Jung YS, Lim JE, Jung JW, Moon JA, Byun MK, Kim YS, Kim SK, Chang J, Lee KK, Park MS. A case of Henoch-Shönlein Purpura caused by rifampin. Tuberc Respir Dis. 2008. 65:116–120.8. Girling DJ, Hitze KL. Adverse reactions to rifampicin. Bull World Health Organ. 1979. 57:45–49.9. Tan WC, Ong CK, Kang SC, Razak MA. Two years review of cutaneous adverse drug reaction from first line anti-tuberculous drugs. Med J Malaysia. 2007. 62:143–146.10. Parish WE, Rhodes EL. Bacterial antigens and aggregated gamma globulin in the lesions of nodular vasculitis. Br J Dermatol. 1967. 79:131–147.11. Johnson NM, McNicol MW, Burton-Kee EJ, Mowbray JF. Circulating immune complexes in tuberculosis. Thorax. 1981. 36:610–617.12. Barbagallo J, Tager P, Ingleton R, Hirsch RJ, Weinberg JM. Cutaneous tuberculosis: diagnosis and treatment. Am J Clin Dermatol. 2002. 3:319–328.13. Poole G, Stradling P, Worlledge S. Potentially serious side effects of high-dose twice-weekly rifampicin. Br Med J. 1971. 3:343–347.14. Schaberg T, Rebhan K, Lode H. Risk factors for side-effects of isoniazid, rifampin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur Respir J. 1996. 9:2026–2030.15. Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med. 2003. 167:1472–1477.16. Kim SH, Lee BH, Lee KD, Park JS, Kim YS, Jee YK, Kim SH, Park HS, Min KU. The prevalence of adverse drug reactions to a short course anti-tuberculosis regimen. Korean J Med. 2007. 73:496–502.17. Ribi C, Hauser C. Adverse reactions to pyrazinamide. Allergy. 2002. 57:964–965.18. Perdu D, Lavaud F, Prevost A, Deschamps F, Cambie MP, Bongrain E, Barhoum K, Kalis B. Erythema multiforme due to pyrazinamide. Allergy. 1996. 51:340–342.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Leukocytoclastic Vasculitis Associated with Pulmonary Tuberculosis
- Cutaneous Leukocytoclastic Vasculitis with Gastrointestinal Involvement after Anti-Tuberculosis Treatment
- Warfarin-induced Leukocytoclastic Vasculitis
- A Case of Leukocytoclastic Vasculitis Following COVID-19 Vaccination
- A Case of Thrombocytopenia and Purpura Induced by Rifamnpin, Pyrazinamide, and Ciprofloxacin