Korean J Crit Care Med.
2015 Aug;30(3):212-217. 10.4266/kjccm.2015.30.3.212.
Successful Immunoglobulin Treatment in Severe Cryptogenic Organizing Pneumonia Caused by Dermatomyositis
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
- 2Division of Pulmonology, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. jwsohn@hanyang.ac.kr
- KMID: 2227652
- DOI: http://doi.org/10.4266/kjccm.2015.30.3.212
Abstract
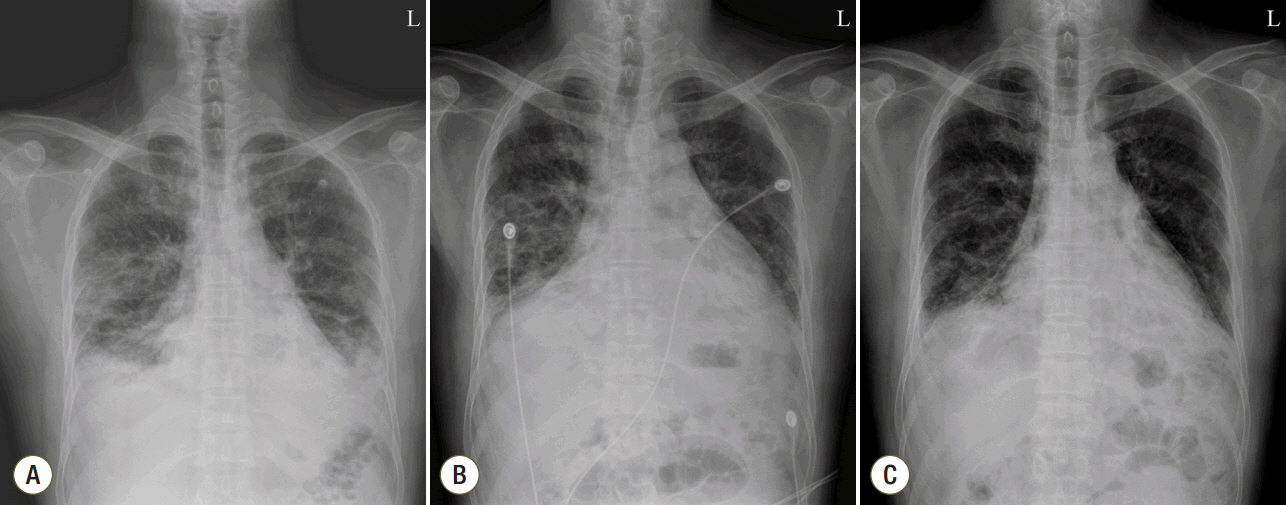
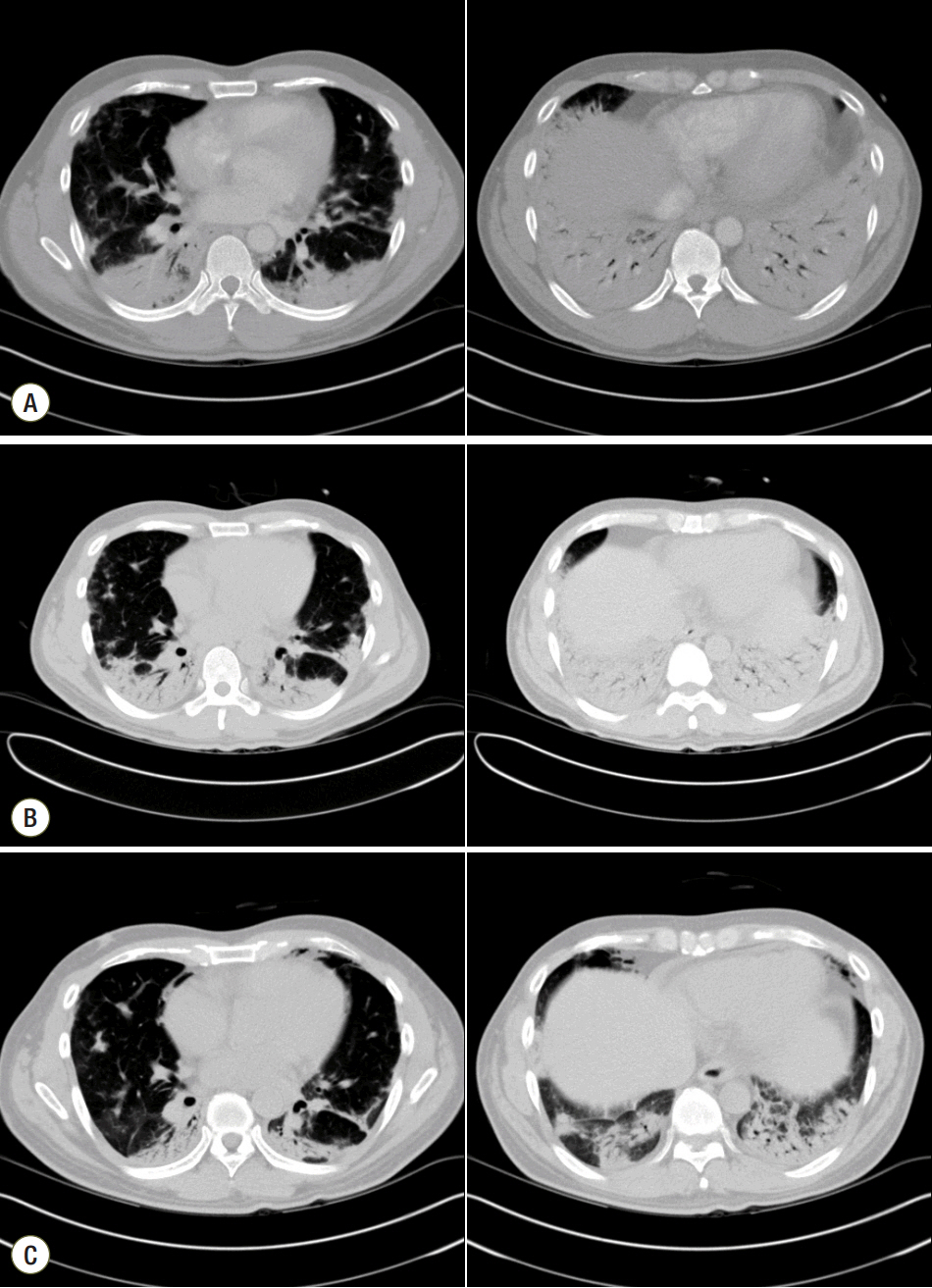
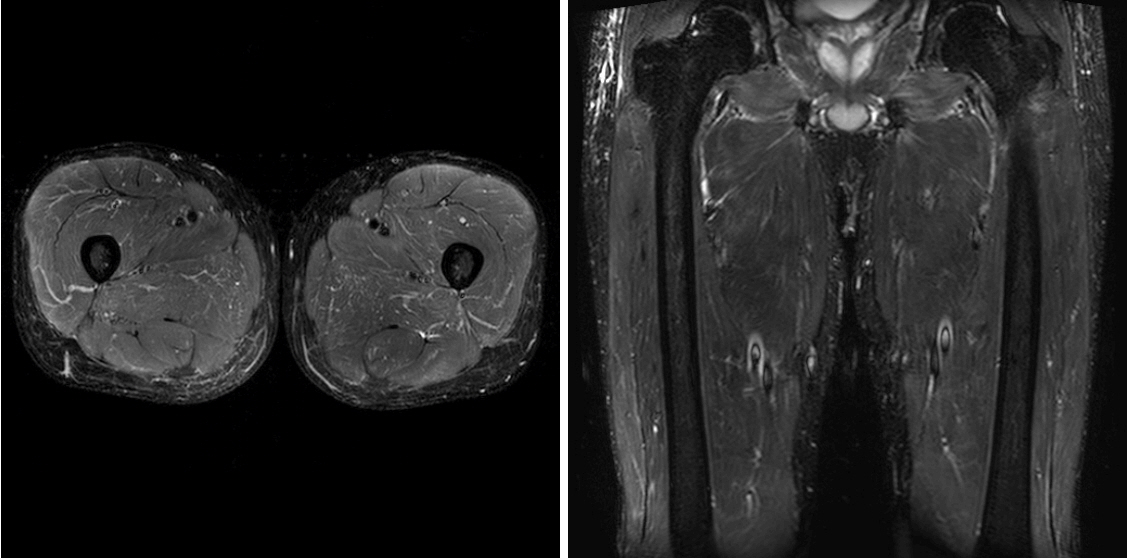
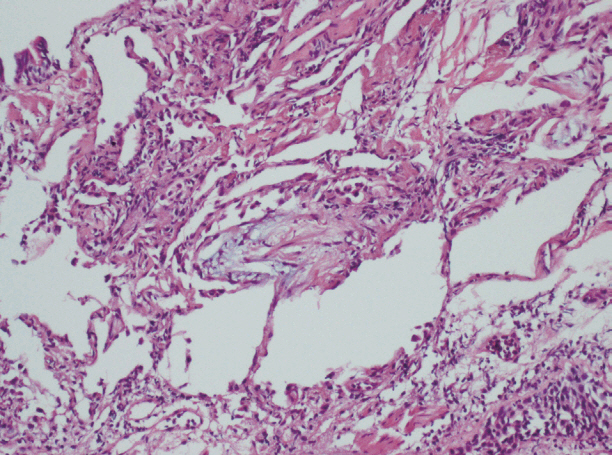
- In connective tissue diseases, autoantibodies cause pulmonary interstitial inflammation and fibrosis, and patients require treatment with an immunosuppressive agent such as a steroid. Dermatomyositis is an incurable, uncommon form of connective tissue disease that occasionally causes diffuse pulmonary inflammation leading to acute severe respiratory failure. In such cases, the prognosis is very poor despite treatment with high-dose steroid. In the present case, a 46-year-old man was admitted to our hospital with dyspnea. He was diagnosed with dermatomyositis combined with cryptogenic organizing pneumonia (COP) with respiratory failure and underwent treatment with steroid and an immunosuppressive agent, but the COP was not improved. However, the respiratory failure did improve after treatment with intravenous immunoglobulin, which therefore can be considered a treatment option in cases where steroids and immunosuppressive agents are ineffective.
Keyword
MeSH Terms
-
Autoantibodies
Connective Tissue Diseases
Cryptogenic Organizing Pneumonia*
Dermatomyositis*
Dyspnea
Fibrosis
Humans
Immunoglobulins*
Immunosuppressive Agents
Inflammation
Lung Diseases, Interstitial
Middle Aged
Pneumonia
Prognosis
Respiratory Insufficiency
Steroids
Autoantibodies
Immunoglobulins
Immunosuppressive Agents
Steroids
Figure
Reference
-
References
1. Bohan A, Peter JB. Polymyositis and dermatomyositis (second of two parts). N Engl J Med. 1975; 292:403–7.2. Keir GJ, Maher TM, Ming D, Abdullah R, de Lauretis A, Wickremasinghe M, et al. Rituximab in severe, treatment-refractory interstitial lung disease. Respirology. 2014; 19:353–9.
Article3. Brulhart L, Waldburger JM, Gabay C. Rituximab in the treatment of antisynthetase syndrome. Ann Rheum Dis. 2006; 65:974–5.
Article4. Keir GJ, Maher TM, Hansell DM, Denton CP, Ong VH, Singh S, et al. Severe interstitial lung disease in connective tissue disease: rituximab as rescue therapy. Eur Respir J. 2012; 40:641–8.
Article5. Suzuki Y, Hayakawa H, Miwa S, Shirai M, Fujii M, Gemma H, et al. Intravenous immunoglobulin therapy for refractory interstitial lung disease associated with polymyositis/dermatomyositis. Lung. 2009; 187:201–6.
Article6. Castelino FV, Varga J. Interstitial lung disease in connective tissue diseases: evolving concepts of pathogenesis and management. Arthritis Res Ther. 2010; 12:213.
Article7. Douglas WW, Tazelaar HD, Hartman TE, Hartman RP, Decker PA, Schroeder DR, et al. Polymyositis-dermatomyositis-associated interstitial lung disease. Am J Respir Crit Care Med. 2001; 164:1182–5.
Article8. Marie I, Hachulla E, Chérin P, Dominique S, Hatron PY, Hellot MF, et al. Interstitial lung disease in polymyositis and dermatomyositis. Arthritis Rheum. 2002; 47:614–22.
Article9. Purcell IF, Bourke SJ, Marshall SM. Cyclophosphamide in severe steroid-resistant bronchiolitis obliterans organizing pneumonia. Respir Med. 1997; 91:175–7.
Article10. Cohen AJ, King TE Jr, Downey GP. Rapidly progressive bronchiolitis obliterans with organizing pneumonia. Am J Respir Crit Care Med. 1994; 149:1670–5.
Article11. Fathi M, Lundberg IE, Tornling G. Pulmonary complications of polymyositis and dermatomyositis. Semin Respir Crit Care Med. 2007; 28:451–8.
Article12. Ando K, Motojima S, Doi T, Nagaoka T, Kaneko N, Aoshima M, et al. Effect of glucocorticoid monotherapy on pulmonary function and survival in Japanese patients with scleroderma-related interstitial lung disease. Respir Investig. 2013; 51:69–75.
Article13. Horai Y, Isomoto E, Koga T, Okada A, Kawashiri SY, Tamai M, et al. Early diagnosis and treatment for remission of clinically amyopathic dermatomyositis complicated by rapid progress interstitial lung disease: a report of two cases. Mod Rheumatol. 2013; 23:190–4.
Article14. Kameda H, Nagasawa H, Ogawa H, Sekiguchi N, Takei H, Tokuhira M, et al. Combination therapy with corticosteroids, cyclosporin A, and intravenous pulse cyclophosphamide for acute/subacute interstitial pneumonia in patients with dermatomyositis. J Rheumatol. 2005; 32:1719–26.15. Danieli M, Malcangi G, Palmieri C, Logullo F, Salvi A, Piani M, et al. Cyclosporin A and intravenous immunoglobulin treatment in polymyositis/dermatomyositis. Ann Rheum Dis. 2002; 61:37–41.
Article16. Bakewell C.J, Raghu G. Polymyositis associated with severe interstitial lung disease: remission after three doses of IV immunoglobulin. Chest. 2011; 139:441–3.17. Miyazaki E, Ando M, Muramatsu T, Fukami T, Matsuno O, Nureki S, et al. Early assessment of rapidly progressive interstitial pneumonia associated with amyopathic dermatomyositis. Clin Rheumatol. 2007; 26:436–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Dermatomyositis with Secondary Organizing Pneumonia
- Dermatomyositis without elevation of creatine kinase presented as bronchiolitis obliterans organizing pneumonia
- A Case of Cryptogenic Organizing Pneumonia after Transarterial Chemoembolization for the Treatment of Hepatocellular Carcinoma
- Korean Guidelines for Diagnosis and Management of Interstitial Lung Diseases: Part 4. Cryptogenic Organizing Pneumonia
- Development of bronchiolitis obliterans organizing pneumonia during standard treatment of hepatitis C with Peg-IFNα2b