Korean J Crit Care Med.
2016 Feb;31(1):63-67. 10.4266/kjccm.2016.31.1.63.
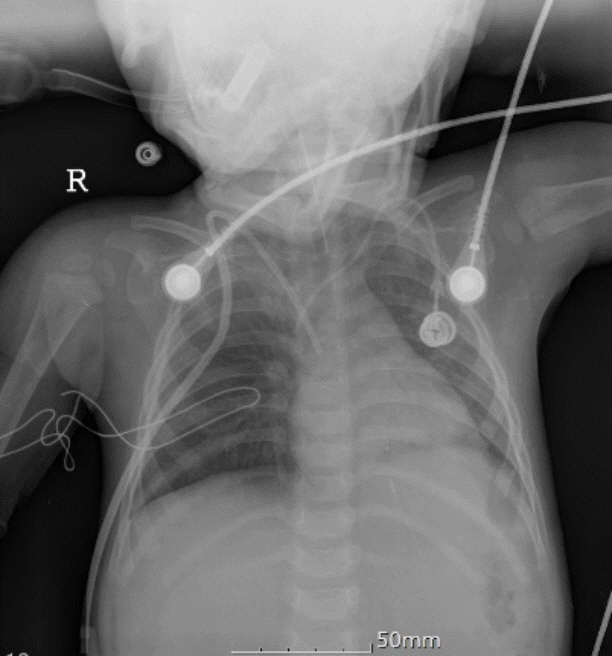
Suspected Pulmonary Embolism during Hickman Catheterization in a Child: What Else Should Be Considered besides Pulmonary Embolism?
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, College of Medicine, Yeungnam University, Daegu, Korea. hmlee@yu.ac.kr
- 2Department of Thoracic Surgery, College of Medicine, Yeungnam University, Daegu, Korea.
- KMID: 2227616
- DOI: http://doi.org/10.4266/kjccm.2016.31.1.63
Abstract
- A 16-month-old girl with acute lymphoblastic leukemia expired during Hickman catheter insertion. She had undergone chemoport insertion of the left subclavian vein six months earlier and received five cycles of chemotherapy. Due to malfunction of the chemoport and the consideration of hematopoietic stem cell transplantation, insertion of a Hickmann catheter on the right side and removal of the malfunctioning chemoport were planned under general anesthesia. The surgery was uneventful during catheter insertion, but the patient experienced the sudden onset of pulseless electrical activity just after saline was flushed through the newly inserted catheter. Cardiopulmonary resuscitation was commenced aggressively, but the patient was refractory. Migration of a thrombus generated by the previous central catheter to the pulmonary circulation was suspected, resulting in a pulmonary embolism.
MeSH Terms
Figure
Reference
-
References
1. Biss TT, Brandão LR, Kahr WH, Chan AK, Williams S. Clinical features and outcome of pulmonary embolism in children. Br J Haematol. 2008; 142:808–18.
Article2. van Ommen CH, Heijboer H, Büller HR, Hirasing RA, Heijmans HS, Peters M. Venous thromboembolism in childhood: a prospective two-year registry in The Netherlands. J Pediatr. 2001; 139:676–81.
Article3. Monagle P, Chan AK, Goldenberg NA, Ichord RN, Journeycake JM, Nowak-Göttl U, et al. Antithrombotic therapy in neonates and children: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e737S–801S.4. Vidal E, Sharathkumar A, Glover J, Faustino EV. Central venous catheter-related thrombosis and thromboprophylaxis in children: a systematic review and meta-analysis. J Thromb Haemost. 2014; 12:1096–109.
Article5. Derish MT, Smith DW, Frankel LR. Venous catheter thrombus formation and pulmonary embolism in children. Pediatr Pulmonol. 1995; 20:349–54.
Article6. Verso M, Agnelli G. Venous thromboembolism associated with long-term use of central venous catheters in cancer patients. J Clin Oncol. 2003; 21:3665–75.
Article7. Higgerson RA, Lawson KA, Christie LM, Brown AM, McArthur JA, Totapally BR, et al. Incidence and risk factors associated with venous thrombotic events in pediatric intensive care unit patients. Pediatr Crit Care Med. 2011; 12:628–34.
Article8. Krafte-Jacobs B, Sivit CJ, Mejia R, Pollack MM. Catheter-related thrombosis in critically ill children: comparison of catheters with and without heparin bonding. J Pediatr. 1995; 126:50–4.
Article9. Male C, Chait P, Ginsberg JS, Hanna K, Andrew M, Halton J, et al. Comparison of venography and ultrasound for the diagnosis of asymptomatic deep vein thrombosis in the upper body in children: results of the PARKAA study. Prophylactic antithrombin replacement in kids with aLL treated with asparaginase. Thromb Haemost. 2002; 87:593–8.10. Massicotte MP, Dix D, Monagle P, Adams M, Andrew M. Central venous catheter related thrombosis in children: analysis of the Canadian Registry of Venous Thromboembolic Complications. J Pediatr. 1998; 133:770–6.
Article11. Nifong TP, McDevitt TJ. The effect of catheter to vein ratio on blood flow rates in a simulated model of peripherally inserted central venous catheters. Chest. 2011; 140:48–53.
Article12. Male C, Chait P, Andrew M, Hanna K, Julian J, Mitchell L, PARKAA Investigators. Central venous line-related thrombosis in children: association with central venous line location and insertion technique. Blood. 2003; 101:4273–8.
Article13. Atchison CM, Arlikar S, Amankwah E, Ayala I, Barrett L, Branchford BR, et al. Development of a new risk score for hospital-associated venous thromboembolism in noncritically ill children: findings from a large single-institutional case-control study. J Pediatr. 2014; 165:793–8.
Article14. Weg JG. A new niche for end-tidal CO2 in pulmonary embolism. Crit Care Med. 2000; 28:3752–4.15. Stockwell MA, Bruce W, Soni N. The influence of CO2 production and physiological deadspace on end-tidal CO2 during controlled ventilation: a study using a mechanical model. Anaesth Intensive Care. 1989; 17:482–6.16. Wiegand UK, Kurowski V, Giannitsis E, Katus HA, Djonlagic H. Effectiveness of end-tidal carbon dioxide tension for monitoring thrombolytic therapy in acute pulmonary embolism. Crit Care Med. 2000; 28:3588–92.17. Bailén MR, Cuadra JAR, Aguayo De Hoyos E. Thrombolysis during cardiopulmonary resuscitation in fulminant pulmonary embolism: a review. Crit Care Med. 2001; 29:2211–9.
Article18. Pavlovic G, Banfi C, Tassaux D, Peter RE, Licker MJ, Bendjelid K, et al. Peri-operative massive pulmonary embolism management: is veno-arterial ECMO a therapeutic option? Acta Anaesthesiol Scand. 2014; 58:1280–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Use of Thrombolytics for Massive Pulmonary Embolism by a Comparison of Cases
- Pulmonary Embolism Associated with Total Hip Replacement for the Fracture of Femur Neck
- Pulmonary Embolism and Pulmonary Infarction
- Acute Massive Pulmonary Thromboembolism Occupying both Whole Pulmonary Arteries
- Acute Pulmonary Embolism