Korean Circ J.
2007 Apr;37(4):154-160. 10.4070/kcj.2007.37.4.154.
Comparison of Efficacy and Safety after Administering High Potency Statin to High Risk Patients: Rosuvastatin 10 mg versus Atorvastatin 20 mg
- Affiliations
-
- 1Department of Cardiovascular Medicine, Wonkwang University Hospital, Iksan, Korea. jjwcar@wonkwang.ac.kr
- 2Department of Neurology, Wonkwang University Hospital, Iksan, Korea.
- KMID: 2227072
- DOI: http://doi.org/10.4070/kcj.2007.37.4.154
Abstract
-
BACKGROUND AND OBJECTIVES: Although the rate of prescribing hydroxylmethyglutaryl-CoA reductase inhibitors (statin) has recently increased, there is a large treatment gap between the guidelines and actual clinical practice. We studied the effect of high potency statin on the percentage of patients who achieve the target low density lipoprotein (LDL) cholesterol level, and we determined the changes of lipid profiles with using 10 mg of rosuvastatin and 20 mg of atorvastatin.
MATERIALS AND METHODS
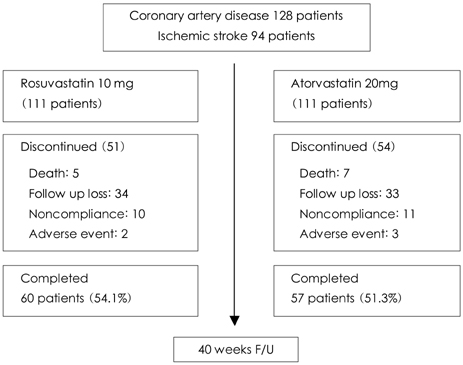
222 consecutive patients with acute coronary syndrome or acute ischemic stroke were randomly assigned to either the group treated with rosuvastatin 10 mg (Group I) or atorvastatin 20 mg (Group II). We compared the percentage of patients who achieved the target LDL cholesterol level, and the percent change of the serum lipid profile from baseline to the 40th week between the two groups.
RESULTS
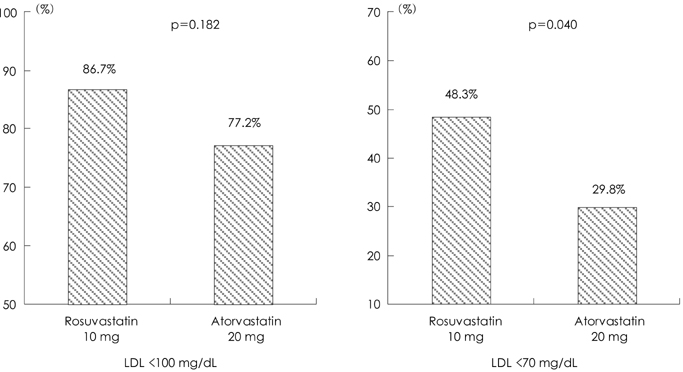
117 (52.7%) patients completed this study. When the target LDL cholesterol level was <100 mg/dL, there was no significant difference in the target attainment rate between the two groups (86.7% vs. 77.2%; respectively, p=0.182). When the target LDL cholesterol level was <70 mg/dL, 48.3% of Group I and 29.8% of Group II reached the goal (p=0.040). The LDL cholesterol level was reduced by 46.8% in Group I (p<0.001), and by 40.1% in Group II (p<0.001). However, the final level showed a trend to be lower in the rosuvastatin group (p=0.077). There were no serious side effects in both groups. The study drug was discontinued due to adverse events in 2 patients (2.6%) of Group I, and in 3 patients (3.8%) of Group II (p=0.523).
CONCLUSION
This study showed that the reduction of LDL cholesterol was not statistically different between rosuvastatin 10 mg and atorvastatin 20 mg. However, fewer than half of the patients achieved the goal in both groups despite of high potency statin therapy. This suggests that more aggressive statin therapy is preferred for high risk patients.
MeSH Terms
Figure
Cited by 1 articles
-
Cholesterol Lowering Effects of Low-dose Statins in Korean Patients
Jee Eun Kwon, Young Kim, Seonghyup Hyun, Hoyoun Won, Seung Yong Shin, Kwang Je Lee, Sang-Wook Kim, Tae Ho Kim, Chee Jeong Kim
J Lipid Atheroscler. 2014;3(1):21-28. doi: 10.12997/jla.2014.3.1.21.
Reference
-
1. Sacandinavian Simvastatin Survival Study (4S). Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease. Lancet. 1994. 344:1383–1389.2. Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia: west of Scotland cornary prevention study group. N Engl J Med. 1995. 333:1301–1307.3. Kim CJ. In the shadow of the statin festival. Korean Circ J. 2006. 36:77–83.4. Long-Term Intervention with Pravastatin in Ischemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients of coronary heart disease and a board range of initial cholesterol levels. N Engl J Med. 1998. 339:1349–1357.5. Jukema JW, Bruschke AV, van Boven AJ, et al. Effects of lipid lowering by pravastatin on progression and regression of coronary artery disease in symptomatic men with normal to moderately elevated serum cholesterol levels. Circulation. 1995. 91:2528–2540.6. Nissen SE, Tuzcu EM, Schoenhagen P, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial. JAMA. 2004. 291:1071–1080.7. Okazaki S, Yokoyama T, Miyauchi K, et al. Early statin treatment in patients with acute coronary syndrome: demonstration of the beneficial effect on atherosclerotic lesions by serial volumetric intravascular ultrasound analysis during half a year after coronary event. Circulation. 2004. 110:1061–1068.8. Yokoi H, Nobuyoshi M, Mitsudo K, Kawaguchi A, Yamamoto A. Three-year follow-up results of angiographic intervention trial using an HMG-CoA reductase inhibitor to evaluate retardation of obstructive multiple atheroma (ATHEROMA) study. Circ J. 2005. 69:875–883.9. Nissen SE, Nicholls SJ, Sipahi I, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis. JAMA. 2006. 295:1556–1565.10. Kim SH, Park JS, Zo JH, Kim MA, Kim HS. Treatment gap in the management of hypercholesterolemia in Korea: return on expenditure achieved for lipid therapy (REALITY). Korean Circ J. 2006. 36:593–599.11. Pearson TA, Peters TD. The treatment gap in coronary artery disease and heart failure: community standards and the post-discharge patients. Am J Cardiol. 1997. 80:45H–52H.12. Pearson TA, Laurora I, Chu H, Kafonek S. The lipid treatment assessment project (L-TAP). Arch Intern Med. 2000. 160:459–467.13. Jones PH, Davidson MH, Stein EA, et al. Comparison of the efficacy and safety of rosuvastatin versus atorvastatin, simvastatin, and provastatin across doses (STELLAR trial). Am J Cardiol. 2003. 92:152–160.14. Friedewald WT, Levy RI, Frederickson DS. Estimation of concentration of low density lipoprotein cholesterol in plasma, without the use of preparative ultracentrifuge. Clin Chem. 1972. 18:499–502.15. West of Scotland Coroanry Prevention Study. Influence of pravastatin and plasma lipids on clinical events in the West of Scotland Coronary Prevention Study (WOSCOPS). Circulation. 1998. 97:1440–1445.16. Shepherd J, Blauw GJ, Murphy MB, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER) : a randomised controlled trial. Lancet. 2002. 360:1623–1630.17. Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high risk individuals: a randomised placebo-controlled trial. Lancet. 2002. 360:7–22.18. Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004. 350:1495–1504.19. Larosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005. 352:1425–1435.20. de Lemos JA, Blazing MA, Wiviott SD, et al. Early intensive vs. a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. JAMA. 2004. 292:1307–1316.21. Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004. 110:227–239.22. Smith SC Jr, Feldman TE, Hirshfeld JW Jr, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention. J Am Coll Cardiol. 2006. 47:e1–e121.23. Kostner GM, Gavish D, Leopold B, Bolzano K, Weintraub MS, Breslow JL. HMG-CoA reductase inhibitors lower LDL cholesterol without reducing Lp(a) levels. Circulation. 1989. 80:1313–1319.24. Maron DJ, Fazio S, Linton MF. Current perspectives on statins. Circulation. 2000. 101:207–213.25. Tekin A, Tekin G, Guzelsoy D, et al. Effects of atorvastatin (10 mg) on hemostatic and inflammatory parameters in hyperlipidemic patients with angiographically ptoven coronary artery disease. Am J Cardiol. 2004. 94:206–209.26. Jones P, Kafonek S, Laurora I, Hunninghake D. Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (the CURVES study). Am J Cardiol. 1998. 81:582–587.27. Schneck DW, Knopp RH, Ballantyne CM, McPherson R, Chitra RR, Simonson SG. Comparative effects of rosuvastatin and atorvastatin across their dose ranges in patients with hypercholesterolemia and without active arterial disease. Am J Cardiol. 2003. 91:33–41.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Efficacy of High-Dose Rosuvastatin and Atorvastatin in Preventing Cystatin C-Oriented Contrast-Induced Nephropathy in Patients With Acute Myocardial Infarction: RACCOON-AMI Registry
- Early efficacy and safety of statin therapy in Korean patients with hypercholesterolemia: Daegu and Gyeongbuk Statin Registry
- Economic Evaluation of Rosuvastatin and Atorvastatin for the Treatment of Dyslipidemia from a Korean Health System Perspective
- Cost-effectiveness of the Use of Statins in the Korean Population
- Efficacy of Moderate Intensity Statins in the Treatment of Dyslipidemia in Korean Patients with Type 2 Diabetes Mellitus