Korean Circ J.
2009 Aug;39(8):322-327. 10.4070/kcj.2009.39.8.322.
Age is an Independent Risk Factor for the Early Morning Blood Pressure Surge in Patients Never-Treated for Hypertension
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. limsh@catholic.ac.kr
- KMID: 2225682
- DOI: http://doi.org/10.4070/kcj.2009.39.8.322
Abstract
- BACKGROUND AND OBJECTIVES
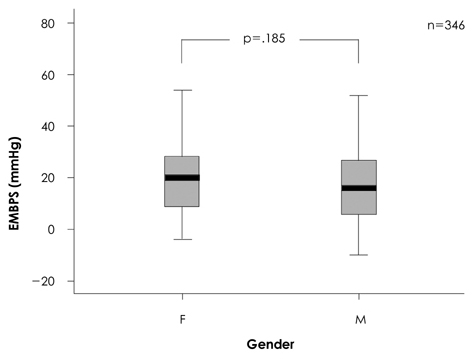
The early morning blood pressure surge (EMBPS) has been reported to be associated with cardiovascular events. The aim of this study was to investigate the relationship between 24-hour ambulatory BP monitoring (ABPM) parameters and conventional cardiovascular risk factors. SUBJECTS AND METHODS: Patients (n=346) never-treated for essential hypertension with no other cardiovascular risk factors, such as diabetes, dyslipidemia, and nephropathy were enrolled. The EMBPS was defined as the early morning systolic BP minus the lowest night systolic BP. We compared the 24-hour ABPM parameters in two groups divided by age (<60 and > or =60 years) and examined the association between the 24-hour ABPM parameters and cardiovascular risk factor. RESULTS: The EMBPS (18+/-14 vs. 24+/-14 mmHg, p=0.002), 24-hour mean blood pressure {MBP; 102+/-9 vs. 105+/-11 mmHg, p=0.044}, and 24-hour mean pulse pressure (PP; 52+/-10 vs. 58+/-11 mmHg, p<0.001) were significantly increased in the elderly subjects compared to the younger subjects. The degree of decrease was less in the elderly subjects (10+/-8 vs. 7+/-10%, p=0.002). Based on multivariate analysis, age was an independent risk factor for the highest quartile of EMBPS (>28 mmHg) after adjusting for gender differences, body mass index, and various 24-hour ABPM parameters (odds ratio, 1.051; 95% confidence interval, 1.028-1.075; p<0.001). CONCLUSION: Age is an independent risk factor for EMBPS in patients with never-treated hypertension. BP control in the early morning period is more important in elderly patients so as to prevent cardiovascular events.
MeSH Terms
Figure
Reference
-
1. Verdecchia P, Clement D, Fagard R, Palatini P, Parati G. Blood Pressure Monitoring. Task Force III. Target organ damage, morbidity and mortality. Blood Press Monit. 1999. 4:303–317.2. Mancia G, Zanchetti A, Agabiti-Rosei E, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. Circulation. 1997. 95:1464–1470.3. Millar-Craig MW, Bishop CN, Raftery EB. Circadian variation of blood pressure. Lancet. 1978. 1:795–797.4. Kario K. Caution for winter morning surge in blood pressure: a possible link with cardiovascular risk in the elderly. Hypertension. 2006. 47:139–140.5. Tofler GH, Brezinski D, Schafer AI, et al. Concurrent morning increase in platelet aggregability and the risk of myocardial infarction and sudden cardiac death. N Engl J Med. 1987. 316:1514–1518.6. Anwar YA, White WB. Chronotherapeutics for cardiovascular disease. Drugs. 1998. 55:631–643.7. Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med. 2003. 348:2407–2415.8. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002. 360:1903–1913.9. Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? Circulation. 2001. 103:1245–1249.10. Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003. 107:1401–1406.11. Elliott WJ. Circadian variation in the timing of stroke onset: a meta-analysis. Stroke. 1998. 29:992–996.12. Cohen MC, Rohtla KM, Lavery CE, Muller JE, Mittleman MA. Meta-analysis of the morning excess of acute myocardial infarction and sudden cardiac death. Am J Cardiol. 1997. 79:1512–1516.13. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003. 42:1206–1252.14. Williams B, Poulter NR, Brown MJ, et al. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): summary. BMJ. 2004. 328:634–640.15. European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003. 21:1011–1053.16. O'Brien E, Asmar R, Beilin L, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003. 21:821–848.17. O'Brien E, Scheridan J, O'Malley K. Dippers and non-dippers. Lancet. 1988. 2:397.18. Najjar SS, Scuteri A, Lakatta EG. Arterial aging: is it an immutable cardiovascular risk factor? Hypertension. 2005. 46:454–462.19. Franklin SS. Pulse pressure as a risk factor. Clin Exp Hypertens. 2004. 26:645–652.20. Laurent S, Katsahian S, Fassot C, et al. Aortic stiffness is an independent predictor of fatal stroke in essential hypertension. Stroke. 2003. 34:1203–1206.21. Laurent S, Boutouyrie P, Asmar R, et al. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001. 37:1236–1241.22. Khattar RS, Swales JD, Dore C, Senior R, Lahiri A. Effect of aging on the prognostic significance of ambulatory systolic, diastolic, and pulse pressure in essential hypertension. Circulation. 2001. 104:783–789.23. Kaneda R, Kario K, Hoshide S, Umeda Y, Hoshide Y, Shimada K. Morning blood pressure hyper-reactivity is an independent predictor for hypertensive cardiac hypertrophy in a community-dwelling population. Am J Hypertens. 2005. 18:1528–1533.24. Zakopoulos NA, Tsivgoulis G, Barlas G, et al. Time rate of blood pressure variation is associated with increased common carotid artery intima-media thickness. Hypertension. 2005. 45:505–512.25. Kario K. Time for focus on morning hypertension: pitfall of current antihypertensive medication. Am J Hypertens. 2005. 18:149–151.26. Kim CH. Ambulatory blood pressure monitoring. Korean Circ J. 1997. 27:1218–1221.27. Lee SM, Kang HS, Song JS, et al. Study of 24 hour ambulatory blood pressure monitoring in acute stroke patients. Korean Circ J. 1999. 29:1212–1218.28. Jeon HC, Kim YK, Kim KY, et al. Determinants of left ventricular mass in healthy adults: a study using echocardiography and 24 hour ambulatory blood pressure monitiring. Korean Circ J. 1995. 25:811–819.29. Head GA, Reid CM, Shiel LM, Jennings GL, Lukoshkova EV. Rate of morning increase in blood pressure is elevated in hypertensives. Am J Hypertens. 2006. 19:1010–1017.30. Kario K. Morning surge and variability in blood pressure: a new therapeutic target? Hypertension. 2005. 45:485–486.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Microbleeds are Associated with Nocturnal Hypertension in Hypertensive Stroke Patients
- Time to First Cigarette and Hypertension in Korean Male Smokers
- Correlation between the morning hypertension on ambulatory blood pressure monitoring and the left ventricular mass in children
- Stroke Update: Optimal Blood Pressure Management for Stroke Prevention
- Morning blood pressure surge in the early stage of hypertensive patients impacts three-dimensional left ventricular speckle tracking echocardiography