Korean Circ J.
2009 Sep;39(9):367-371. 10.4070/kcj.2009.39.9.367.
Prognosis and Natural History of Drug-Related Bradycardia
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea. choyk@knu.ac.kr
- 2Department of Internal Medicine, Gumi CHA Hospital, Gumi, Korea.
- 3Department of Internal Medicine, Masan Samsung Medical Center, Masan, Korea.
- 4Department of Internal Medicine, College of Medicine, Kosin University, Busan, Korea.
- 5Department of Internal Medicine, Daegu Catholic University Hospital, Daegu, Korea.
- 6Department of Internal Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea.
- KMID: 2225672
- DOI: http://doi.org/10.4070/kcj.2009.39.9.367
Abstract
- BACKGROUND AND OBJECTIVES
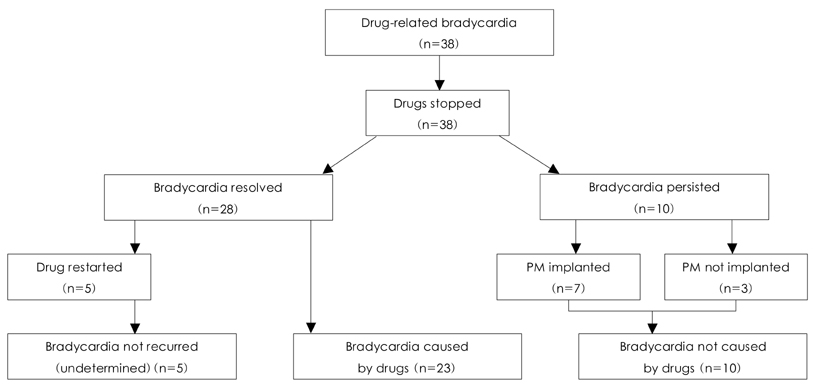
The prognosis and natural history of bradycardia related to drugs such as beta-blockers and non-dihydropyridine calcium channel blockers are not well known. SUBJECTS AND METHODS: We retrospectively analyzed 38 consecutive patients (age 69+/-11, 21 women) with drug-related bradycardia (DRB) between March 2005 and September 2007. A drug-associated etiology for the bradycardia was established based on the medical history and patient response to drug discontinuation. The mean follow-up duration was 18+/-8 months. RESULTS: The initial electrocardiogram (ECG) showed sinus bradycardia (heart rate < or =40/min) in 13 patients, sinus bradycardia with junctional escape beats in 18 patients, and third-degree atrioventricular (AV) block in seven patients. Drug discontinuation was followed by resolution of bradycardia in 60% of patients (n=23). Among them, five (17.8%) patients resumed taking the culprit medication after discharge and none developed bradycardia again. Bradycardia persisted in 10 (26.3%) patients despite drug withdrawal, and a permanent pacemaker was implanted in seven of them. Third-degree AV block, QRS width, and bradycardia requiring temporary transvenous pacing were significantly associated with the bradycardia caused by drugs. CONCLUSION: Beta-blockers were the most common drugs associated with DRB. However, in one quarter of the cases the DRB was not associated with drugs; in these patients permanent pacemaker implantation should be considered.
Keyword
MeSH Terms
Figure
Reference
-
1. Gregoratos G, Abrams J, Epstein AE, et al. ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practical Guidelines (ACC/AHA/NASPE Committee to Update the 1988 Pacemaker Guidelines). Circulation. 2002. 106:2145–2161.2. Gupta AK, Maheshwari A, Tresch DD, Thakur RK. Cardiac arrhythmias in the elderly. Card Electrophysiol Rev. 2002. 6:120–128.3. Mangrum JM, DiMarco JP. The evaluation and management of bradycardia. N Engl J Med. 2000. 342:703–709.4. Shohat-Zabarski R, Iakobishvili Z, Kusniec J, Mazur A, Strasberg B. Paroxysmal atrioventricular block: clinical experience with 20 patients. Int J Cardiol. 2004. 97:399–405.5. López-sedón J, Swedberg K, McMurray J, et al. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004. 25:1341–1362.6. Ovysyshcher IE, Barold SS. Drug-induced bradycardia: to pace or not to pace? Pacing Clin Electrophysiol. 2004. 27:1144–1147.7. Zeltser D, Justo D, Halkin A, et al. Drug-induced atrioventricular block: prognosis after discontinuation of the culprit drug. J Am Coll Cardiol. 2004. 44:105–108.8. Edoute Y, Nagachandran P, Svirski B, Ben-Ami H. Cardiovascular adverse drug reaction associated with combined beta-adrenergic and calcium entry-blocking agents. J Cardiovasc Pharmacol. 2000. 35:556–559.9. Hauser TH, Pinto DS, Josephson ME, Zimetbaum P. Safety and feasibility of a clinical pathway for the outpatient initiation of antiarrhythmic medications in patients with atrial fibrillation or atrial flutter. Am J Cardiol. 2003. 91:1437–1441.10. Essebag V, Hadjis T, Platt RW, Pilote L. Amiodarone and the risk of bradyarrhythmia requiring permanent pacemaker in elderly patients with atrial fibrillation and prior myocardial infarction. J Am Coll Cardiol. 2003. 41:249–254.11. Maisel WH, Kuntz K, Reimond S, et al. Risk of initiating antiarrhythmic drug therapy for atrial fibrillation in patients admitted to a university hospital. Ann Intern Med. 1997. 127:281–284.12. Friedman PL, Stevenson WG. Proarrhythmia. Am J Cardiol. 1998. 82:50N–58N.13. Kenneback G, Tabrizi F, Lindell P, Nordlander R. High-degree atrioventricular block during anti-arrhythmic drug treatment: use of a pacemaker with a bradycardia-detection algorithm to study the time course after drug withdrawal. Europace. 2007. 9:186–191.14. Hjalmarson A, Goldstein S, Fagerberg B, et al. Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure. JAMA. 2000. 283:1295–1302.15. Krum H, Roecker EB, Mohacsi P, et al. Effects of initiating carvedilol in patients with severe chronic heart failure: results from the COPERNICUS Study. JAMA. 2003. 289:712–718.16. Cho YJ, Lee MM, Choe SJ, et al. A randomized, double-blind clinical trial to determine the efficacy of carvedilol vs. atenolol in patients with stage 1 to 2 essential hypertension. Korean Circ J. 1998. 28:359–365.17. Cha DH, Cha YS, Kook JH, et al. Clinical efficacy of carvedilol in patients with moderate to severe congestive heart failure. Korean Circ J. 1998. 26:523–531.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Natural History of Untreated Early Gastric Cancer
- Treatment response and disease progression
- Korean Traditional Medicines as Novel Drugs for Neuropsychiatric Disorders
- Natural History of Chronic Urticaria in Korea
- IgG4-Related Sclerosing Cholangitis Showing Natural Course of Progression to Decompensated Liver Cirrhosis