Korean Circ J.
2010 Dec;40(12):616-624. 10.4070/kcj.2010.40.12.616.
The Impact of Circadian Variation on 12-Month Mortality in Patients With Acute Myocardial Infarction
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea. choyk@mail.knu.ac.kr
- 2Department of Internal Medicine, Gumi Cha Hospital, Gumi, Korea.
- 3Department of Internal Medicine, Busan St. Mary's Medical Center, Busan, Korea.
- KMID: 2225159
- DOI: http://doi.org/10.4070/kcj.2010.40.12.616
Abstract
- BACKGROUND AND OBJECTIVES
Although circadian variation in the onset of acute myocardial infarction (AMI) has been reported in a number of studies, not much is known about the impact of circadian variation on 12-month mortality. The aim of this study was to investigate the impact of circadian variation on 12-month mortality in patients with AMI.
SUBJECTS AND METHODS
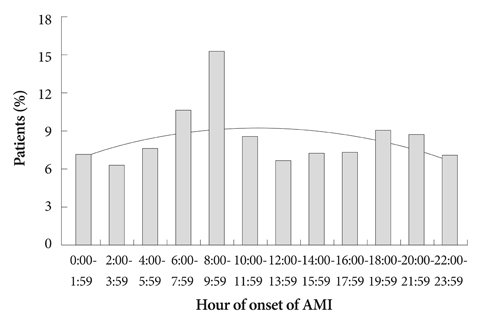
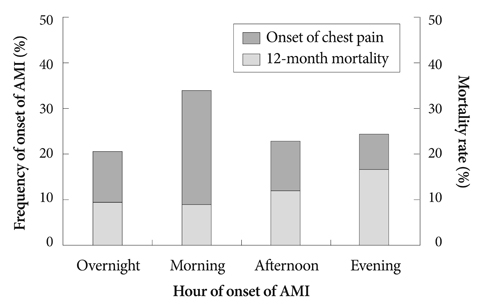
Eight hundred ninety two patients (mean age 67+/-12; 66.1% men) with AMI who visited Kyungpook National University Hospital from November 2005 to December 2007 were included in this study. Patients were divided into groups based on four 6-hours intervals: overnight (00:00-05:59); morning (06:00-11:59); afternoon (12:00-17:59) and evening (18:00-23:59).
RESULTS
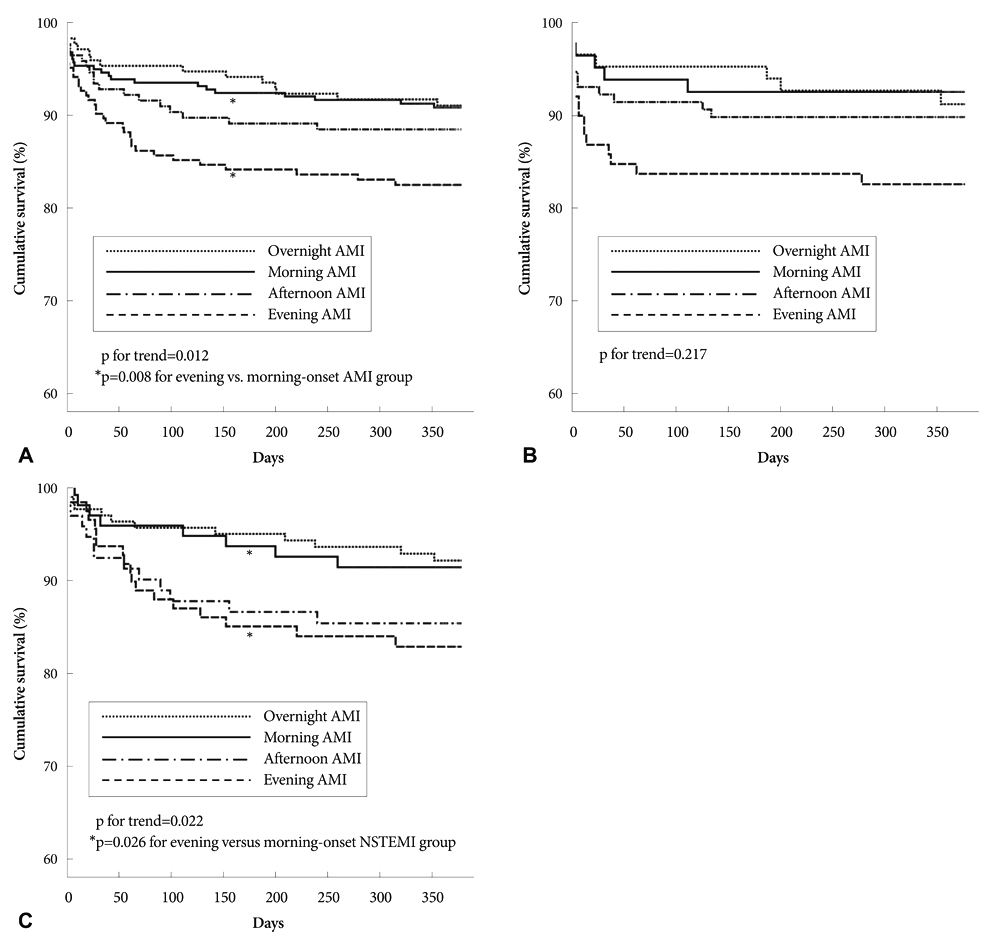
Kaplan-Meier survival curves showed 12-month mortality rates of 9.6%, 9.1%, 12.1%, and 16.7% in the overnight, morning, afternoon, evening-onset groups, respectively (p=0.012). Compared with the morning-onset AMI group, the serum creatinine levels (p=0.002), frequency of Killip class > or =3 (p=0.004), and prescription rate of diuretics (p=0.011) were significantly higher in the evening-onset AMI group, while the left ventricular ejection fraction (p=0.012) was significantly lower. The proportion of patients who arrived in the emergency room during routine duty hours was significantly lower in evening-onset groups irrespective of the presence or absence of ST-segment elevation (p<0.001). According to univariate analysis, the 12-month mortality rate in the evening group was significantly higher compared to the morning group (hazard ratio 1.998, 95% confidence interval 1.196 to 3.338, p=0.008).
CONCLUSION
Patients with evening-onset AMI had poorer baseline clinical characteristics, and this might affect the circadian impact on 12-month mortality. Further studies are needed to clarify the role of circadian variation on the long-term outcome of AMI.
Keyword
MeSH Terms
Figure
Reference
-
1. Kinoshita N, Imai K, Kinjo K, Naka M. Longitudinal study of acute myocardial infarction in the southeast Osaka district from 1988 to 2002. Circ J. 2005. 69:1170–1175.2. Hjalmarson A, Gilpin EA, Nicod P, et al. Differing circadian patterns of symptom onset in subgroups of patients with acute myocardial infarction. Circulation. 1989. 80:267–275.3. Kim KS, Song YS, Hur SH, et al. Circadian variation in acute myocardial infarction. Korean Circ J. 1993. 23:173–183.4. López F, Lee KW, Marín F, et al. Are there ethnic differences in the circadian variation in onset of acute myocardial infarction?: a comparison of 3 ethnic groups in Birmingham, UK and Alicante, Spain. Int J Cardiol. 2005. 100:151–154.5. D'Negri CE, Nicola-Siri L, Vigo DE, Girotti LA, Cardinali DP. Circadian analysis of myocardial infarction incidence in an Argentine and Uruguayan population. BMC Cardiovasc Disord. 2006. 6:1.6. Rana JS, Mukamal KJ, Morgan JP, Muller JE, Mittleman MA. Circadian variation in the onset of myocardial infarction: effect of duration of diabetes. Diabetes. 2003. 52:1464–1468.7. Kinjo K, Sato H, Sato H, et al. Circadian variation of the onset of acute myocardial infarction in the Osaka area, 1998-1999: characterization of morning and nighttime peaks. Jpn Circ J. 2001. 65:617–620.8. Muller JE, Kaufmann PG, Luepker RV, Weisfeldt ML, Deedwania PC, Willerson JT. Mechanisms precipitating acute cardiac events: review and recommendations of an NHLBI workshop. National Heart, Lung, and Blood Institute. Circulation. 1997. 96:3233–3239.9. Bhalla A, Sachdev A, Lehl SS, Singh R, D'Cruz S. Ageing and circadian variation in cardiovascular events. Singapore Med J. 2006. 47:305–308.10. Willich SN. Circadian variation and triggering of cardiovascular events. Vasc Med. 1999. 4:41–49.11. Sari I, Davutoglu V, Erer B, et al. Analysis of circadian variation of acute myocardial infarction: afternoon predominance in Turkish population. Int J Clin Pract. 2009. 63:82–86.12. Henriques JP, Haasdijk AP, Zijlstra F. Outcome of primary angioplasty for acute myocardial infarction during routine duty hours versus during off-hours. J Am Coll Cardiol. 2003. 41:2138–2142.13. Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA. 2005. 294:803–812.14. Mukamal KJ, Muller JE, Maclure M, Sherwood JB, Mittleman MA. Increased risk of congestive heart failure among infarctions with nighttime onset. Am Heart J. 2000. 140:438–442.15. Park SR, Kang YR, Seo MK, et al. Clinical predictors of incomplete ST-segment resolution in the patients with acute ST segment elevation myocardial infarction. Korean Circ J. 2009. 39:310–316.16. Lee CH, Joo SJ, Park DS, et al. Remodeling and changes of systolic and diastolic functions of left ventricle after acute myocardial infarction: comparison according to killip class at admission. Korean Circ J. 1998. 28:1727–1739.17. Al Suwaidi J, Reddan DN, Williams K, et al. Prognostic implications of abnormalities in renal function in patients with acute coronary syndromes. Circulation. 2002. 106:974–980.18. Naidu SS, Selzer F, Jacobs A, et al. Renal insufficiency is an independent predictor of mortality after percutaneous coronary intervention. Am J Cardiol. 2003. 92:1160–1164.19. Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000. 283:2941–2947.20. Magid DJ, Calonge BN, Rumsfeld JS, et al. Relation between hospital primary angioplasty volume and mortality for patients with acute MI treated with primary angioplasty vs thrombolytic therapy. JAMA. 2000. 284:3131–3138.21. Canto JG, Every NR, Magid DJ, et al. The volume of primary angioplasty procedures and survival after acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. N Engl J Med. 2000. 342:1573–1580.22. Vakili BA, Kaplan R, Brown DL. Volume-outcome relation for physicians and hospitals performing angioplasty for acute myocardial infarction in New York state. Circulation. 2001. 104:2171–2176.23. Assali AR, Brosh D, Vaknin-Assa H, et al. The impact of circadian variation on outcomes in emergency acute anterior myocardial infarction percutaneous coronary intervention. Catheter Cardiovasc Interv. 2006. 67:221–226.24. Dominguez-Rodriguez A, Garcia-Gonzalez M, Abreu-Gonzalez P. Outcome of primary angioplasty for ST-segment elevation myocardial infarction during routine duty hours versus during off-hours: results of a single-center in Spain. Int J Cardiol. 2007. 119:227–229.25. Berger PB, Ellis SG, Holmes DR Jr, et al. Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes (GUSTO-IIb) Trial. Circulation. 1999. 100:14–20.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Circadian and Seasonal Variations in the Frequency of Onset of Acute Myocardial Infarction
- Acute Myocardial Infarction in the Evening Has a Worse Prognosis. Circadian Rhythm, Does It Matter?
- Circadian variation in acute myocardial infarction
- Reproducibility and diurnal variation of heart rate variability in predischarge period of acute myocardial infarction
- Circadian Variation of Ventricular Premature Complex in Hypertension and Ischemic Heart Disease Patients