Korean Circ J.
2012 Aug;42(8):528-537. 10.4070/kcj.2012.42.8.528.
Clinical Characteristics of Acute Aortic Syndrome in Korean Patients: From the Korean Multi-Center Registry of Acute Aortic Syndrome
- Affiliations
-
- 1Cardiology Division, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 2Cardiology Division, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. cdhlyj@yuhs.ac
- 3Cardiology Division, Seoul St. Mary's Hospital, The Catholic University College of Medicine, Seoul, Korea.
- 4Cardiology Division, Kyungpook National University Hospital, Daegu, Korea.
- 5Cardiology Division, Ajou University Medical Center, Suwon, Korea.
- 6Cardiovascular Center, Korea University Anam Hospital, Seoul, Korea.
- 7Cardiology Division, National Health Insurance Coperation Ilsan Hospital, Goyang, Korea.
- 8Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea.
- 9Department of Cardiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 10Cardiology Division, Wonju Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 11Cardiology Division, Chonnam National University Hospital, Gwangju, Korea.
- KMID: 2225002
- DOI: http://doi.org/10.4070/kcj.2012.42.8.528
Abstract
- BACKGROUND AND OBJECTIVES
Acute aortic syndrome (AAS) is a heterogeneous group of disorders that often present with severe chest or back pain. It includes acute aortic dissection (AD), intramural hematoma (IMH), dissecting aneurysm, and penetrating aortic ulcer (PAU). The clinical picture of AAS and its prognosis have not been studied in a large number of Korean patients. Therefore, we organized a multi-center registry to identify the clinical characteristics and treatment patterns, as well as long-term outcomes in Korean patients with AAS.
SUBJECTS AND METHODS
Five-hundred twenty-eight patients, who had been diagnosed with AAS, were enrolled into this registry from 10 centers. On a retrospective basis, we collected demographic, laboratory, imaging data, as well as follow-up clinical outcomes by reviewing medical records from individual centers. All the data were collected in core lab and analyzed in detail.
RESULTS
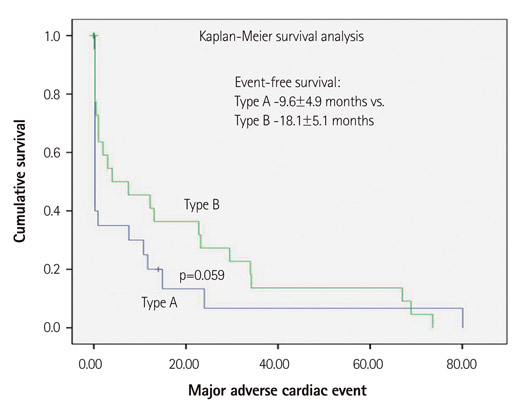
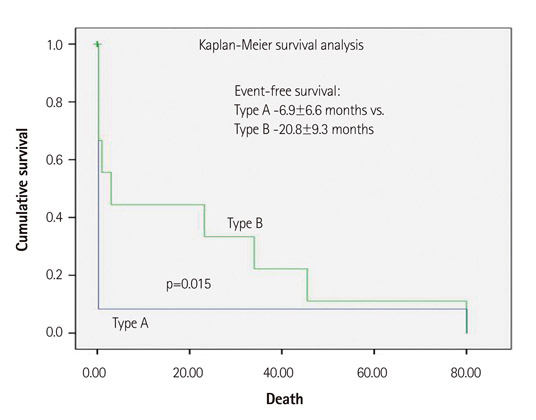
The mean patient age was 60.1+/-14.5 years; the male-to-female ratio was M : F=297 : 231. The prevalent risk factors for AAS included hypertension (361, 68.4%) and diabetes (52, 11.1%). The components of AAS that are included in this study are acute AD (446, 84.5%), IMH (57, 10.7%), and PAU (11, 2.1%). By type of AAS, patients diagnosed with Stanford A were 45.6% of enrolled patients, whereas those with Stanford B were 54.4% of enrolled patients. Among nearly half of the patients were treated with medicine (55.7%) alone, whereas 40.0% underwent surgery and 4.3% underwent endovascular treatment. Overall, the in-hospital event rate was 21.2% and the in-hospital death rate was 8.1%. The mean follow-up duration was 42.8 months and there showed 22.9% of total event and 10.1% of death during this period.
CONCLUSION
By organizing a multi-center registry of AAS, we could identify the characteristics of AAS in real-world Korean patients. Further, prospective study is warranted with a larger number of patients.
MeSH Terms
Figure
Cited by 2 articles
-
Incidence and Mortality Rates of Thoracic Aortic Dissection in Korea – Inferred from the Nationwide Health Insurance Claims
Jun Ho Lee, Yongil Cho, Yang Hyun Cho, Hyunggoo Kang, Tae Ho Lim, Hyo Jun Jang, Sun Kyun Ro, Hyuck Kim
J Korean Med Sci. 2020;35(40):e360. doi: 10.3346/jkms.2020.35.e360.Usefulness of Cardiac Biomarkers in the Evaluation of Prognosis and Cardiac Involvement in Patients with Acute Aortic Syndrome
Jong Yoon Kim, Kye Hun Kim, Yi Rang Yim, Jae Yeong Cho, Doo Sun Sim, Hyun Ju Yoon, Nam Sik Yoon, Young Joon Hong, Hyung Wook Park, Ju Han Kim, Youngkeun Ahn, Myung Ho Jeong, Jeong Gwan Cho, Jong Chun Park
J Lipid Atheroscler. 2016;5(1):27-36. doi: 10.12997/jla.2016.5.1.27.
Reference
-
1. Vilacosta I, Román JA. Acute aortic syndrome. Heart. 2001. 85:365–368.2. Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000. 283:897–903.3. Mehta RH, Suzuki T, Hagan PG, et al. Predicting death in patients with acute type A aortic dissection. Circulation. 2002. 105:200–206.4. Vilacosta I, Aragoncillo P, Cañadas V, San Román JA, Ferreirós J, Rodríguez E. Acute aortic syndrome: a new look at an old conundrum. Heart. 2009. 95:1130–1139.5. Coady MA, Rizzo JA, Elefteriades JA. Pathologic variants of thoracic aortic dissections: penetrating atherosclerotic ulcers and intramural hematomas. Cardiol Clin. 1999. 17:637–657.6. Lansman SL, Saunders PC, Malekan R, Spielvogel D. Acute aortic syndrome. J Thorac Cardiovasc Surg. 2010. 140:6 Suppl. S92–S97.7. Hirst AE Jr, Johns VJ Jr, Kime SW Jr. Dissecting aneurysm of the aorta: a review of 505 cases. Medicine (Baltimore). 1958. 37:217–279.8. Wilson SK, Hutchins GM. Aortic dissecting aneurysms: causative factors in 204 subjects. Arch Pathol Lab Med. 1982. 106:175–180.9. Earnest F 4th, Muhm JR, Sheedy PF 2nd. Roentgenographic findings in thoracic aortic dissection. Mayo Clin Proc. 1979. 54:43–50.10. Cho SH, Sung K, Park KH, et al. Midterm results of aortic arch replacement in a Stanford type A aortic dissection with an intimal tear in the aortic arch. Korean Circ J. 2009. 39:270–274.11. Campbell-Lloyd AJ, Mundy J, Pinto N, et al. Contemporary results following surgical repair of acute type A aortic dissection (AAAD): a single centre experience. Heart Lung Circ. 2010. 19:665–672.12. Mohr-Kahaly S, Erbel R, Kearney P, Puth M, Meyer J. Aortic intramural hemorrhage visualized by transesophageal echocardiography: findings and prognostic implications. J Am Coll Cardiol. 1994. 23:658–664.13. Nienaber CA, von Kodolitsch Y, Petersen B, et al. Intramural hemorrhage of the thoracic aorta: diagnostic and therapeutic implications. Circulation. 1995. 92:1465–1472.14. Song JK, Kim HS, Kang DH, et al. Different clinical features of aortic intramural hematoma versus dissection involving the ascending aorta. J Am Coll Cardiol. 2001. 37:1604–1610.15. Kaji S, Akasaka T, Horibata Y, et al. Long-term prognosis of patients with type A aortic intramural hematoma. Circulation. 2002. 106:12 Suppl 1. I248–I252.16. Evangelista A, Mukherjee D, Mehta RH, et al. Acute intramural hematoma of the aorta: a mystery in evolution. Circulation. 2005. 111:1063–1070.17. Moizumi Y, Komatsu T, Motoyoshi N, Tabayashi K. Management of patients with intramural hematoma involving the ascending aorta. J Thorac Cardiovasc Surg. 2002. 124:918–924.18. Song JK, Yim JH, Ahn JM, et al. Outcomes of patients with acute type A aortic intramural hematoma. Circulation. 2009. 120:2046–2052.19. Kang WC, Joung BY, Ko YG, et al. Favorable outcome of endovascular stent-graft implantation for Stanford type B aortic dissection. Korean Circ J. 2003. 33:457–464.20. Botsios S, Schuermann K, Maatz W, Keck N, Walterbusch G. Complicated acute type B dissections: a single-center experience with endovascular treatment. Thorac Cardiovasc Surg. 2010. 58:280–284.21. Lee S, Kim W, Hwang SH, et al. The relationship of inflammatory reaction with the mortality of type B acute aortic syndrome. Korean Circ J. 2006. 36:387–392.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Placement of Endovascular Stent Graft in Acute Malperfusion Syndrome After Acute Type II Aortic Dissection
- Update on Acute Aortic Syndrome
- Acute Aortic Syndrome: Recent Trends in Imaging Assessment Using Computed Tomography Angiography
- A Case of Acute Aortic Dissection Presenting with Chest Pain Relieved by Sublingual Nitroglycerin
- Acute Type II Aortic Dissection with Severe Aortic Regurgitation and Chronic Descending Aortic Dissection in Pregnant Patient with Marfan Syndrome