Korean Circ J.
2013 May;43(5):343-346. 10.4070/kcj.2013.43.5.343.
Successful Prasugrel Rescue Therapy in Clopidogrel Resistant Patients Who Had Recurrent Stent Thrombosis of Drug-Eluting-Stent: The Role of Prasugrel in Clopidogrel Nonresponders
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. mkhong61@yuhs.ac
- 2Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2224933
- DOI: http://doi.org/10.4070/kcj.2013.43.5.343
Abstract
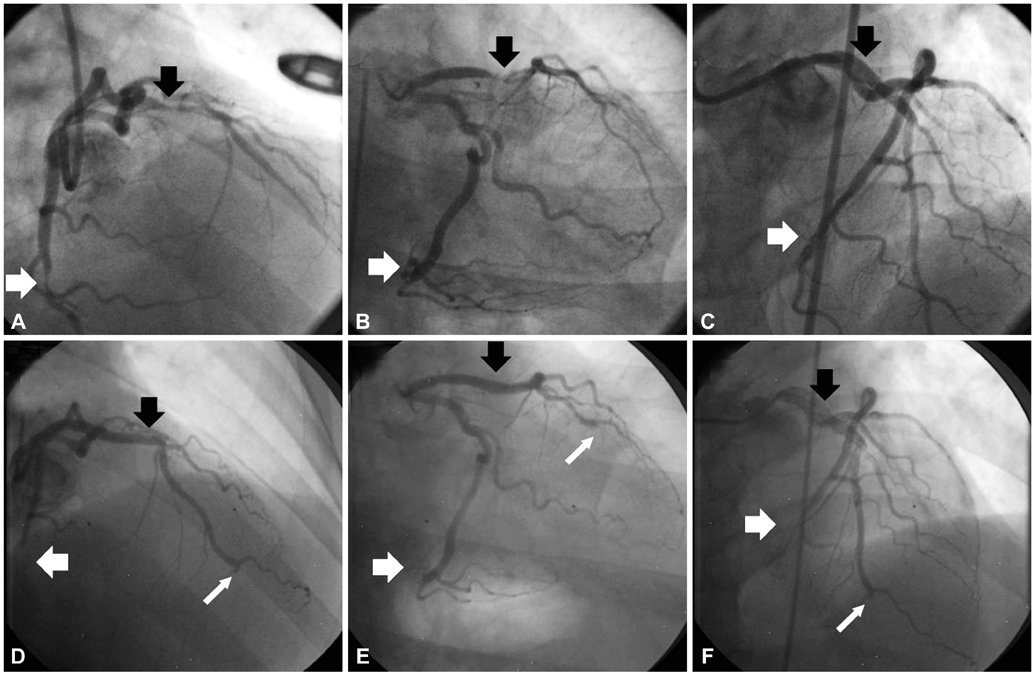
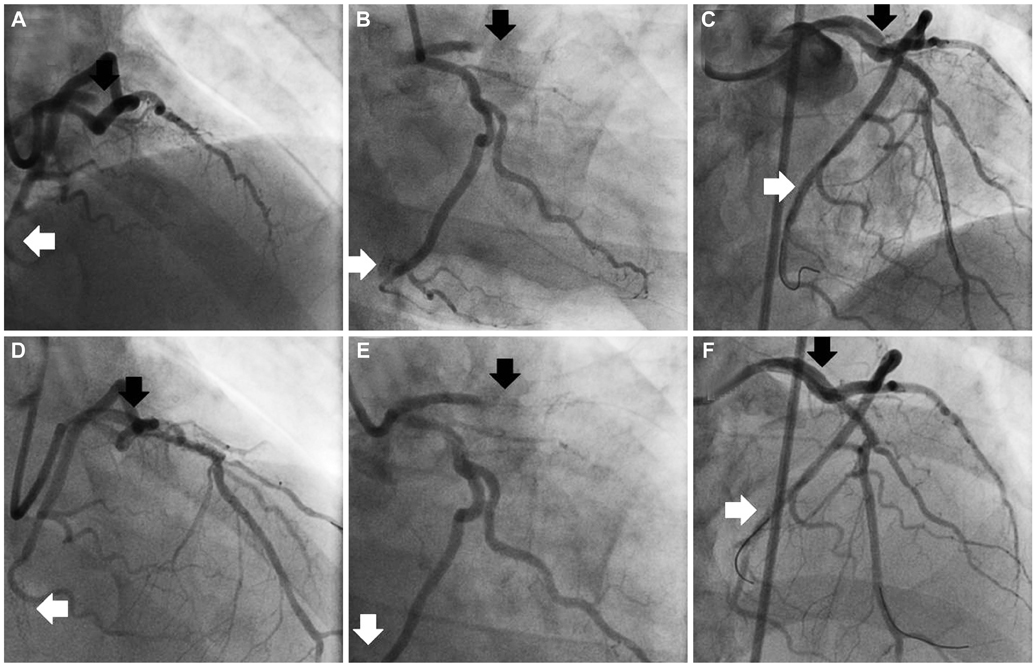
- Stent thrombosis is a very serious problem after drug-eluting stent (DES) implantation even though its incidence is about or less than 1%. As the clopidogrel resistance is expected to play an important role in the occurrence of stent thrombosis, new anti-platelet agents overcoming this issue can give us another choice. We experienced a case of a 58-year-old male with successful prasugrel rescue therapy in a patient with clopidogrel resistance who had recurrent stent thrombosis following DES implantation.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Role of Novel Oral Anticoagulants and Antiplatelet Therapy after Percutaneous Coronary Intervention: Individualizing Therapy to Optimize Outcomes
Evan Shlofmitz, Richard Shlofmitz, Michael S. Lee
Korean Circ J. 2019;49(8):645-656. doi: 10.4070/kcj.2019.0185.
Reference
-
1. Daemen J, Wenaweser P, Tsuchida K, et al. Early and late coronary stent thrombosis of sirolimus-eluting and paclitaxel-eluting stents in routine clinical practice: data from a large two-institutional cohort study. Lancet. 2007; 369:667–678.2. Honda Y, Fitzgerald PJ. Stent thrombosis: an issue revisited in a changing world. Circulation. 2003; 108:2–5.3. Antman EM, Wiviott SD, Murphy SA, et al. Early and late benefits of prasugrel in patients with acute coronary syndromes undergoing percutaneous coronary intervention: a TRITON-TIMI 38 (TRial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet InhibitioN with Prasugrel-Thrombolysis In Myocardial Infarction) analysis. J Am Coll Cardiol. 2008; 51:2028–2033.4. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, et al. Identification of low responders to a 300-mg clopidogrel loading dose in patients undergoing coronary stenting. Thromb Res. 2005; 115:101–108.5. Gurbel PA, Tantry US. Drug insight: Clopidogrel nonresponsiveness. Nat Clin Pract Cardiovasc Med. 2006; 3:387–395.6. Serebruany VL, Steinhubl SR, Berger PB, Malinin AI, Bhatt DL, Topol EJ. Variability in platelet responsiveness to clopidogrel among 544 individuals. J Am Coll Cardiol. 2005; 45:246–251.7. Wright RS, Anderson JL, Adams CD, et al. 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the American Academy of Family Physicians, Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2011; 57:e215–e367.8. Price MJ, Berger PB, Teirstein PS, et al. Standard- vs high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention: the GRAVITAS randomized trial. JAMA. 2011; 305:1097–1105.9. Douglas JS Jr, Holmes DR Jr, Kereiakes DJ, et al. Coronary stent restenosis in patients treated with cilostazol. Circulation. 2005; 112:2826–2832.10. Lee SW, Park SW, Hong MK, et al. Triple versus dual antiplatelet therapy after coronary stenting: impact on stent thrombosis. J Am Coll Cardiol. 2005; 46:1833–1837.11. Rehmel JL, Eckstein JA, Farid NA, et al. Interactions of two major metabolites of prasugrel, a thienopyridine antiplatelet agent, with the cytochromes P450. Drug Metab Dispos. 2006; 34:600–607.12. Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007; 357:2001–2015.13. Jernberg T, Payne CD, Winters KJ, et al. Prasugrel achieves greater inhibition of platelet aggregation and a lower rate of non-responders compared with clopidogrel in aspirin-treated patients with stable coronary artery disease. Eur Heart J. 2006; 27:1166–1173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ticagrelor Rescue Therapy in a Patient with Subacute Stent Thrombosis
- An Intra-procedural Stent Thrombosis in a Prasugrel Resistant Patient Treated with Ticagrelor
- Simultaneous Multivessel Acute Stent Thrombosis in a Patient with Gastrointestinal Bleeding
- Prasugrel-Induced Hypersensitivity Skin Reaction
- Low-Dose Prasugrel in Patients with Resistance to Clopidogrel for the Treatment of Cerebral Aneurysms