Korean Circ J.
2014 Jul;44(4):264-267. 10.4070/kcj.2014.44.4.264.
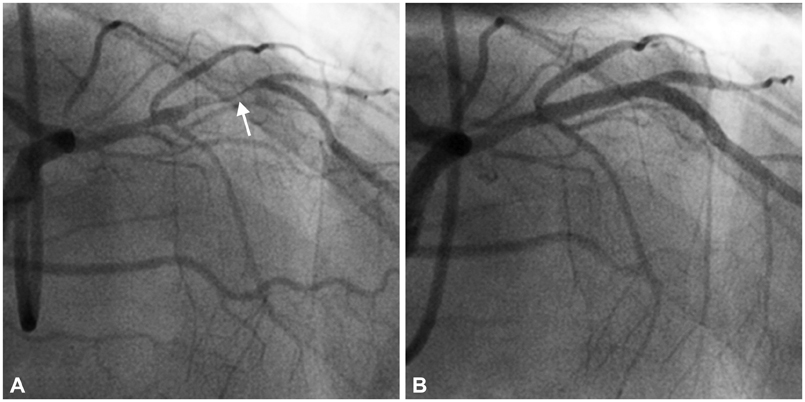
Revascularization for Patients with Idiopathic Thrombocytopenic Purpura and Coronary Artery Disease
- Affiliations
-
- 1Division of Cardiology, Yeungnam University Medical Center, Daegu, Korea. woongwa@hanmail.net
- KMID: 2223888
- DOI: http://doi.org/10.4070/kcj.2014.44.4.264
Abstract
- Idiopathic thrombocytopenic purpura (ITP) is an autoimmune disorder with a low platelet count characterized by premature platelet destruction and suppression of platelet production mediated by autoantibodies, which may predispose to bleeding. Although the prevalence of coronary artery disease (CAD) in ITP seems to be rare, their co-occurrence is not unusual. Patients with ITP have increased risks for thrombosis and atherosclerosis associated with hemostatic factors, endothelial damage, and the negative effects of steroid and immunoglobulin therapies. Thus, the coexistence of ITP and CAD presents complex problems requiring a balance between hemorrhagic risk and prevention of thrombosis. Here, the authors present two patients with ITP, who were revascularized in different ways for CAD. Although the optimal management of thrombocytopenic patients with CAD is uncertain, individualized treatment modalities can be useful in patients with ITP and CAD.
MeSH Terms
Figure
Reference
-
1. Cines DB, Bussel JB, Liebman HA, Luning Prak ET. The ITP syndrome: pathogenic and clinical diversity. Blood. 2009; 113:6511–6521.2. Cines DB, Blanchette VS. Immune thrombocytopenic purpura. N Engl J Med. 2002; 346:995–1008.3. Fruchter O, Blich M, Jacob G. Fatal acute myocardial infarction during severe thrombocytopenia in a patient with idiopathic thrombocytopenic purpura. Am J Med Sci. 2002; 323:279–280.4. Paolini R, Zamboni S, Ramazzina E, Zampieri P, Cella G. Idiopathic thrombocytopenic purpura treated with steroid therapy does not prevent acute myocardial infarction: a case report. Blood Coagul Fibrinolysis. 1999; 10:439–442.5. Elkayam O, Paran D, Milo R, et al. Acute myocardial infarction associated with high dose intravenous immunoglobulin infusion for autoimmune disorders. A study of four cases. Ann Rheum Dis. 2000; 59:77–80.6. Khandekar MM, Khurana AS, Deshmukh SD, Kakrani AL, Katdare AD, Inamdar AK. Platelet volume indices in patients with coronary artery disease and acute myocardial infarction: an Indian scenario. J Clin Pathol. 2006; 59:146–149.7. Patrassi GM, Sartori MT, Rigotti P, et al. Coagulation and fibrinolysis during the first year of immunosuppressive treatment in renal transplantation: correspondence between hypercoagulable state and steroid therapy. Clin Appl Thromb Hemost. 1995; 1:277–282.8. Stangel M, Hartung HP, Marx P, Gold R. Side effects of high-dose intravenous immunoglobulins. Clin Neuropharmacol. 1997; 20:385–393.9. Fisman DN, Smilovitch M. Intravenous immunoglobulin, blood viscosity and myocardial infarction. Can J Cardiol. 1997; 13:775–777.10. Caputo RP, Abraham S, Churchill D. Transradial coronary stent placement in a patient with severe idiopathic autoimmune thrombocytopenic purpura. J Invasive Cardiol. 2000; 12:365–368.11. Moretti C, Teresa Lucciola M, Morena L, et al. Idiopathic thrombocytopenic purpura and percutaneous coronary stenting: a dangerous duo? Int J Cardiol. 2008; 130:e96–e97.12. Fong MC, Chen KC, Leu HB, Chen LC. Coronary revascularization in a patient with immune thrombocytopenic purpura. J Chin Med Assoc. 2006; 69:436–438.13. Neskovic AN, Stankovic I, Milicevic P, et al. Primary PCI for acute myocardial infarction in a patient with idiopathic thrombocytopenic purpura. A case report and review of the literature. Herz. 2010; 35:43–49.14. Agostoni P, Biondi-Zoccai GG, de Benedictis ML, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; Systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol. 2004; 44:349–356.15. Russo A, Cannizzo M, Ghetti G, et al. Idiopathic thrombocytopenic purpura and coronary artery disease: comparison between coronary artery bypass grafting and percutaneous coronary intervention. Interact Cardiovasc Thorac Surg. 2011; 13:153–157.16. Chevalier B, Lancelin B, Koning R, et al. Effect of a closure device on complication rates in high-local-risk patients: results of a randomized multicenter trial. Catheter Cardiovasc Interv. 2003; 58:285–291.17. Yellin A, Refaely Y, Paley M, Simansky D. Major bleeding complicating deep sternal infection after cardiac surgery. J Thorac Cardiovasc Surg. 2003; 125:554–558.18. Mathew TC, Vasudevan R, Leb L, Pezzella SM, Pezzella AT. Coronary artery bypass grafting in immune thrombocytopenic purpura. Ann Thorac Surg. 1997; 64:1059–1062.19. Inoue Y, Lim RC, Nand P. Coronary artery bypass grafting in an immune thrombocytopenic purpura patient using off-pump techniques. Ann Thorac Surg. 2004; 77:1819–1821.20. Ascione R, Williams S, Lloyd CT, Sundaramoorthi T, Pitsis AA, Angelini GD. Reduced postoperative blood loss and transfusion requirement after beating-heart coronary operations: a prospective randomized study. J Thorac Cardiovasc Surg. 2001; 121:689–696.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Infarction Associated with Idiopathic Thrombocytopenic Purpura
- Diagnosis and treatment of purpura
- Idiopathic Thrombocytopenic Purpura
- A case of idiopathic thrombocytopenic purpura in pregnancy
- Primary Percutaneous Coronary Intervention for Acute Myocardial Infarction with Idiopathic Thrombocytopenic Purpura: A Case Report