J Rheum Dis.
2015 Feb;22(1):39-44. 10.4078/jrd.2015.22.1.39.
Knee Synovitis Mimicking a Septic Arthritis
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 2Division of Nephrology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Division of Rheumatology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. taeyoung@yonsei.ac.kr
- KMID: 2222926
- DOI: http://doi.org/10.4078/jrd.2015.22.1.39
Abstract
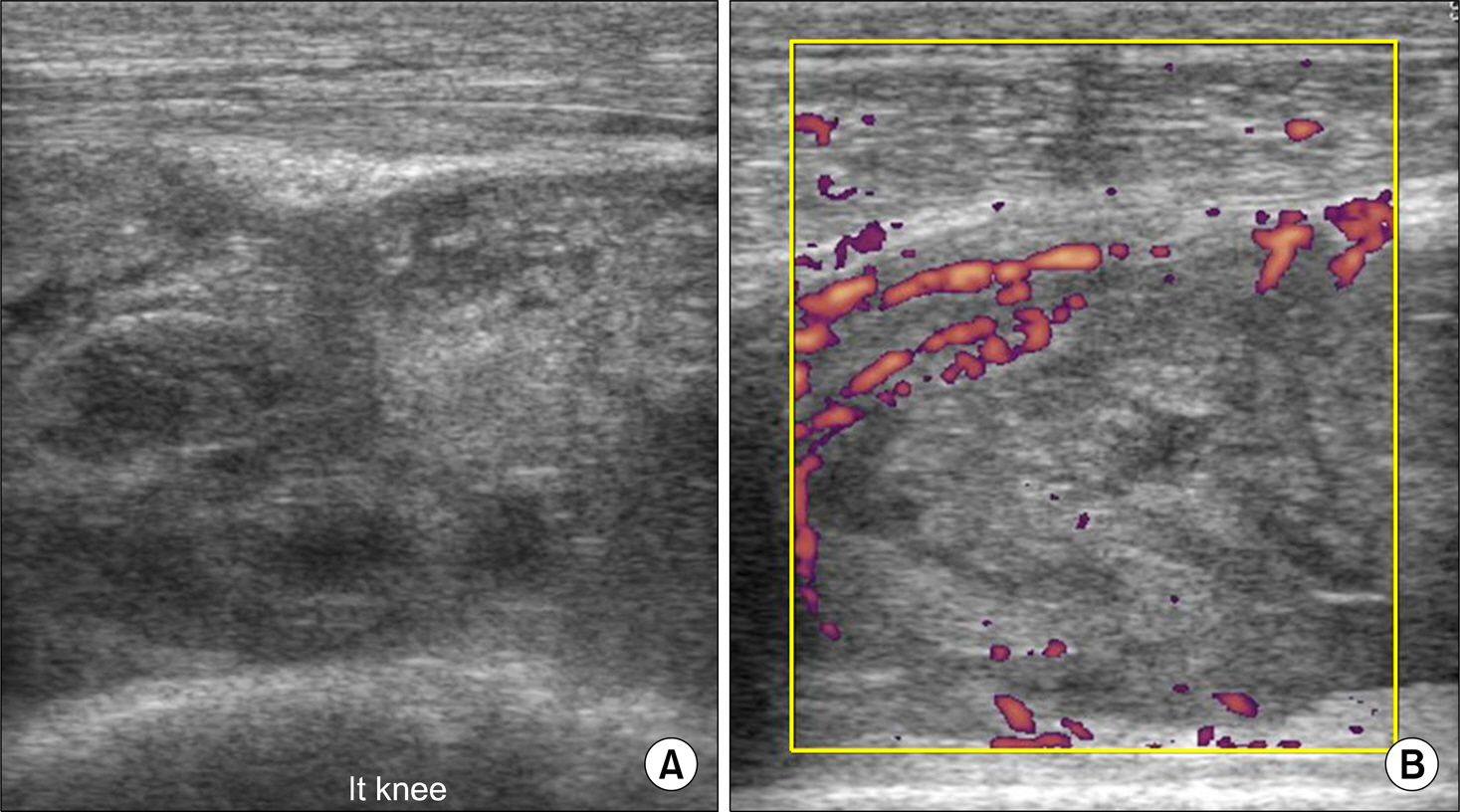
- Synovitis is the inflammation of the synovial membrane with unknown etiology which occurs in association with auto-immune inflammatory arthritis, mainly in rheumatoid arthritis. Synovitis manifesting as rapidly progressing monoarticular or pauciarticualr symptoms could make early diagnosis difficult, thus it could be misdiagnosed as other forms of arthritic diseases. We experienced a rare case of knee joint synovitis which initially manifested as mimicking a septic arthritis. A 58-year-old-male patient underwent renovascular embolization due to retroperitoneal hemorrhage which was developed after renal biopsy. Suddenly, the patient's left knee joint became swollen rapidly with redness and tenderness. Moreover, his right knee also became inflamed. Surgical irrigation and intravenous antibiotics had never worked on his knee joint inflammation, however administration of intermediate dose of steroid could decrease inflammatory signs dramatically. Synovitis in a large joint could be mistaken as a septic arthritis, delaying the right diagnosis. Thus, we report this case with literature review.
Keyword
MeSH Terms
Figure
Reference
-
1. Hitchon CA, El-Gabalawy HS. The synovium in rheumatoid arthritis. Open Rheumatol J. 2011; 5:107–14.2. Morgan DS, Fisher D, Merianos A, Currie BJ. An 18 year clinical review of septic arthritis from tropical Australia. Epidemiol Infect. 1996; 117:423–8.
Article3. Li SF, Cassidy C, Chang C, Gharib S, Torres J. Diagnostic utility of laboratory tests in septic arthritis. Emerg Med J. 2007; 24:75–7.
Article4. American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum. 2002; 46:328–46.5. Landewé RB, Boers M, Verhoeven AC, Westhovens R, van de Laar MA, Markusse HM, et al. COBRA combination therapy in patients with early rheumatoid arthritis: long-term structural benefits of a brief intervention. Arthritis Rheum. 2002; 46:347–56.
Article6. Narváez J, Sirvent E, Narváez JA, Bas J, Gómez-Vaquero C, Reina D, et al. Usefulness of magnetic resonance imaging of the hand versus anticyclic citrullinated peptide antibody testing to confirm the diagnosis of clinically suspected early rheumatoid arthritis in the absence of rheumatoid factor and radiographic erosions. Semin Arthritis Rheum. 2008; 38:101–9.
Article7. Sugimoto H, Takeda A, Hyodoh K. Early-stage rheumatoid arthritis: prospective study of the effectiveness of MR imaging for diagnosis. Radiology. 2000; 216:569–75.
Article8. Szkudlarek M, Court-Payen M, Strandberg C, Klarlund M, Klausen T, Ostergaard M. Power Doppler ultrasonography for assessment of synovitis in the metacarpophalangeal joints of patients with rheumatoid arthritis: a comparison with dynamic magnetic resonance imaging. Arthritis Rheum. 2001; 44:2018–23.
Article9. Merino R, de Inocencio J, García-Consuegra J. Differentiation between transient synovitis and septic arthritis of the hip with clinical and ultrasound criteria. An Pediatr (Barc). 2010; 73:189–93.10. van Gaalen FA, Linn-Rasker SP, van Venrooij WJ, de Jong BA, Breedveld FC, Verweij CL, et al. Autoantibodies to cyclic citrullinated peptides predict progression to rheumatoid arthritis in patients with undifferentiated arthritis: a prospective cohort study. Arthritis Rheum. 2004; 50:709–15.
Article11. Laskari K, Ahmadi-Simab K, Lamken M, Csernok E, Gross WL, Hellmich B. Are anti-cyclic citrullinated peptide autoantibodies seromarkers for rheumatoid vasculitis in a cohort of patients with systemic vasculitis? Ann Rheum Dis. 2010; 69:469–71.
Article12. Kaandorp CJ, Krijnen P, Moens HJ, Habbema JD, van Schaardenburg D. The outcome of bacterial arthritis: a prospective community-based study. Arthritis Rheum. 1997; 40:884–92.
Article13. Dubost JJ, Fis I, Denis P, Lopitaux R, Soubrier M, Ristori JM, et al. Polyarticular septic arthritis. Medicine (Baltimore). 1993; 72:296–310.
Article14. Szkudlarek M, Narvestad E, Klarlund M, Court-Payen M, Thomsen HS, Østergaard M. Ultrasonography of the meta-tarsophalangeal joints in rheumatoid arthritis: comparison with magnetic resonance imaging, conventional radiography, and clinical examination. Arthritis Rheum. 2004; 50:2103–12.
Article15. Rantapää-Dahlqvist S, de Jong BA, Berglin E, Hallmans G, Wadell G, Stenlund H, et al. Antibodies against cyclic citrullinated peptide and IgA rheumatoid factor predict the development of rheumatoid arthritis. Arthritis Rheum. 2003; 48:2741–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pigmented Villonodular Synovitis Developing in the Knee of a Rheumatoid Arthritis Patient Mistaken as a Rheumatoid Arthritis Flare-Up
- A Case of Multiple Rice Bodies by the Nonspecific Synovitis in the Knee Joint
- A Case of Pedunculated Localized Nodular Synovitis of the Knee: MR Imaging Findings
- Arthroscopic Synovectomy on Knee Joint
- Septic Knee Arthritis Caused by Corynebacterium striatum