J Rheum Dis.
2013 Jun;20(3):186-189. 10.4078/jrd.2013.20.3.186.
A Case of Bone Marrow Edema Syndrome in a Patient with Anti-phospholipid Syndrome
- Affiliations
-
- 1Department of Rheumatology, Chonnam National University Medical School, Gwangju, Korea. shinseok@chonnam.ac.kr
- 2Department of Radiology, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 2222759
- DOI: http://doi.org/10.4078/jrd.2013.20.3.186
Abstract
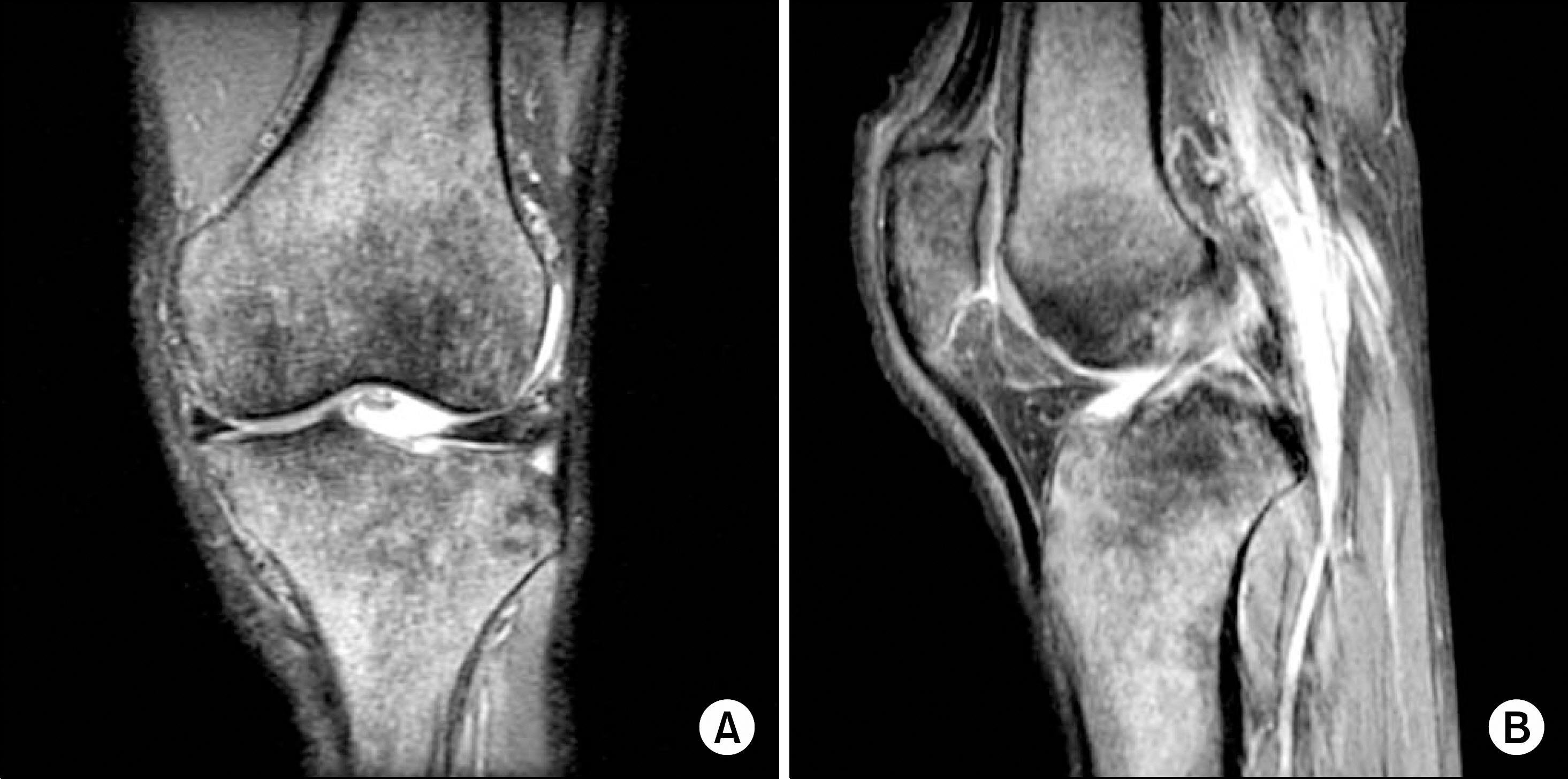
- Bone marrow edema is a common and nonspecific finding on magnetic resonance imaging (MRI) and results from various diseases including infection, inflammation, neoplasm, injury, and osteoarthritis. However, bone marrow edema syndrome (BMES) represents a distinct entity with specific clinical and imaging features such as diffuse extensions, the lack of other morphologic alterations, no history of trauma, and reversible disease courses. BMES is caused by ischemic changes, and thus, it is postulated to occur as a result of the thrombosis in a patient with primary anti-phospholipid syndrome (APS). Here, we present a case of 67-year-old male with a history of stroke, being presented with fever of unknown origin and pain on both knees. He had high titers of IgG and IgM anti-cardiolipin antibodies which titers didn't change after 3 months. He was diagnosed as having a BMES due to typical MRI findings. After the introduction of anticoagulation, fever and joint pain were subsided. Our case suggests that BMES can develop within a patient with APS, thus early detection of differentiations is essential to avoid unnecessary treatments.
MeSH Terms
Figure
Reference
-
References
1. Korompilias AV, Karantanas AH, Lykissas MG, Beris AE. Bone marrow edema syndrome. Skeletal Radiol. 2009; 38:425–36.
Article2. Hofmann S, Kramer J, Vakil-Adli A, Aigner N, Breitenseher M. Painful bone marrow edema of the knee: differential diagnosis and therapeutic concepts. Orthop Clin North Am. 2004; 35:321–33.
Article3. Papadopoulos ECh, Papagelopoulos PJ, Kaseta M, Themistocleous GS, Korres DS. Bone marrow edema syndrome of the knee: a case report and review of the literature. Knee. 2003; 10:295–302.
Article4. Curtiss PH Jr, Kincaid WE. Transitory demineralization of the hip in pregnancy. A report of three cases. J Bone Joint Surg Am. 1959; 41-A:1327–33.5. Guerra JJ, Steinberg ME. Distinguishing transient osteoporosis from avascular necrosis of the hip. J Bone Joint Surg Am. 1995; 77:616–24.
Article6. Rosen RA. Transitory demineralization of the femoral head. Radiology. 1970; 94:509–12.
Article7. Noorda RJ, van der Aa JP, Wuisman PI, David EF, Lips PT, van der Valk P. Transient osteoporosis and osteogenesis imperfecta. A case report. Clin Orthop Relat Res. 1997; 337:249–55.
Article8. O'Hare A, Shortt C, Napier N, Eustace SJ. Bone marrow edema: patterns and clinical implications. Semin Musculoskelet Radiol. 2006; 10:249–57.9. Phan CM, Link TM, Blumenkrantz G, Dunn TC, Ries MD, Steinbach LS, et al. MR imaging findings in the followup of patients with different stages of knee osteoarthritis and the correlation with clinical symptoms. Eur Radiol. 2006; 16:608–18.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bone Marrow Edema Syndrome of the Foot and Ankle in Adolescents
- A Case of Primary Anti-Phospholipid Syndrome with Recurrent Renal Infarction
- Bilateral Bone Marrow Edema Syndrome of the Femoral Head with a Unique Onset: A Case Report
- Bilateral Frosted Branch Angiitis in Anti-phospholipid Antibody Syndrome
- A Case of Histiocytoid Sweet's Syndrome with Myelodysplastic Syndrome