Ann Rehabil Med.
2013 Jun;37(3):453-458. 10.5535/arm.2013.37.3.453.
Flaccid Leg Paralysis Caused by a Thoracic Epidural Catheterization: A Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, Chungbuk National University College of Medicine, Cheongju, Korea. soulover7@hanmail.net
- KMID: 2219547
- DOI: http://doi.org/10.5535/arm.2013.37.3.453
Abstract
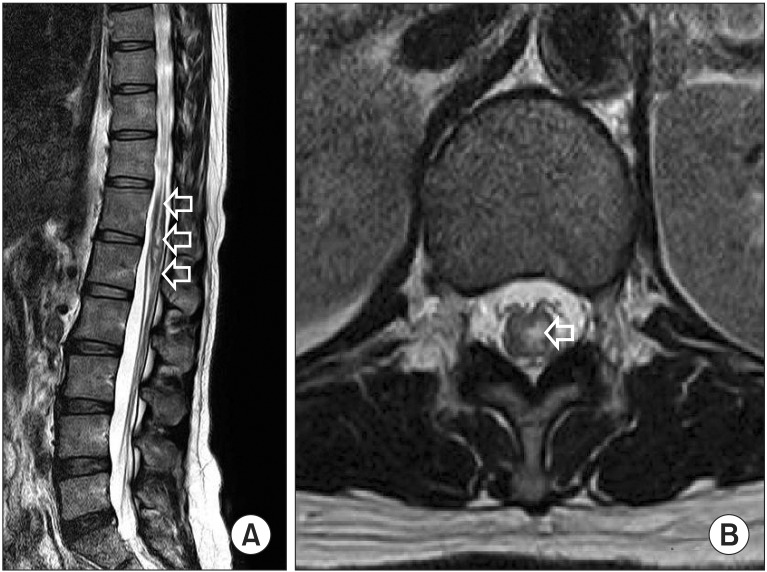
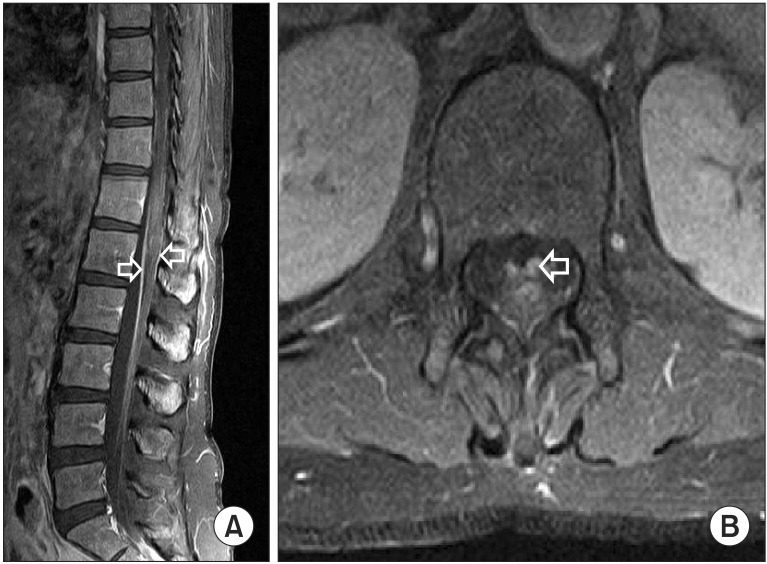
- We report a case of a 44-year-old patient with paralysis of the left leg who had a thoracic epidural catheterization after general anesthesia for abdominal surgery. Sensory losses below T10 and motor weakness of the left leg occurred after the surgery. Magnetic resonance image study demonstrated a well-defined intramedullary linear high signal intensity lesion on T2-weighted image and low-signal intensity on T1-weighted image in the spinal cord between T9 and L1 vertebral level, and enhancements of the spinal cord below T8 vertebra and in the cauda equina. Electrodiagnostic examination revealed lumbosacral polyradiculopathy affecting nerve roots below L4 level on left side. We suggest that the intrinsic spinal cord lesion and nerve root lesion can be caused by an epidural catheterization with subsequent local anesthetic injection.
Keyword
MeSH Terms
Figure
Reference
-
1. Ahn JS, Kim SJ, Kim EG. A case of intrinsic spinal cord lesions complicating epidural anesthesia. J Korean Neurol Assoc. 2006; 24:181–183.2. Wheatley RG, Schug SA, Watson D. Safety and efficacy of postoperative epidural analgesia. Br J Anaesth. 2001; 87:47–61. PMID: 11460813.
Article3. Wilkinson PA, Valentine A, Gibbs JM. Intrinsic spinal cord lesions complicating epidural anaesthesia and analgesia: report of three cases. J Neurol Neurosurg Psychiatry. 2002; 72:537–539. PMID: 11909921.4. Kao MC, Tsai SK, Tsou MY, Lee HK, Guo WY, Hu JS. Paraplegia after delayed detection of inadvertent spinal cord injury during thoracic epidural catheterization in an anesthetized elderly patient. Anesth Analg. 2004; 99:580–583. PMID: 15271743.
Article5. Seo KC, Kim JE, Kim JH, Song SY, Chung JY, Roh WS. Injury to the spinal cord by a thoracic epidural catheter used to control postpneumonectomy pain: a case report. Korean J Anesthesiol. 2009; 56:720–724.6. Ross JS, Moore KR, Shah LM, Borg B, Crim J. Diagnostic imaging: spine. 2nd ed. Altona: Amirsys;2010.7. Jeong JS, Park KD, Lim OK. A case report of persistent cauda equina syndrome following epidural anesthesia. J Korean Assoc EMG Electrodiagn Med. 2009; 11:151–155.8. Han KD, Jeong YJ, Lim SA. Cauda equina syndrome following epidural anesthesia: a case report. Korean J Anesthesiol. 1998; 35:786–790.
Article9. Fischer HB. Regional anaesthesia: before or after general anaesthesia? Anaesthesia. 1998; 53:727–729. PMID: 9797514.10. Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990; 322:1405–1411. PMID: 2278545.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Injury to the spinal cord by a thoracic epidural catheter used to control postpneumonectomy pain : A case report
- Epidural Abscess Following Continuous Epidural Catheterization for the Management of Chronic Cancer Pain: A case report
- Left Leg Paralysis after Lumbar Epidural Block: A case report
- Lower Extremity Paralysis Developed during Pain Control in Lung Cancer Patient: A case report
- Epidural Abscess Secondary to Acute Osteomyelitis of the Cervical Spine Caused by E. coli(A Case Report)