Allergy Asthma Respir Dis.
2016 Jan;4(1):74-78. 10.4168/aard.2016.4.1.74.
Rapid-onset of severe tigecycline-induced coagulopathy in drug reaction with eosinophilia and systemic symptom syndrome
- Affiliations
-
- 1Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 2Department of Allergy and Clinical Immunology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. kwonhs21@naver.com
- KMID: 2218624
- DOI: http://doi.org/10.4168/aard.2016.4.1.74
Abstract
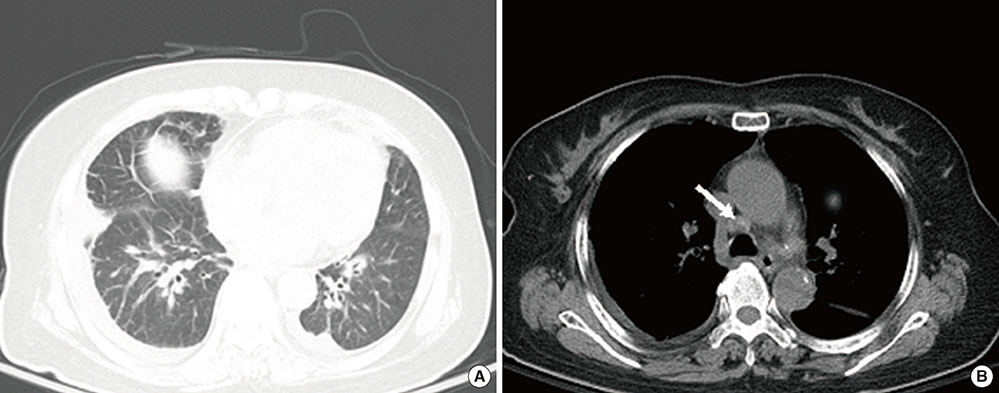
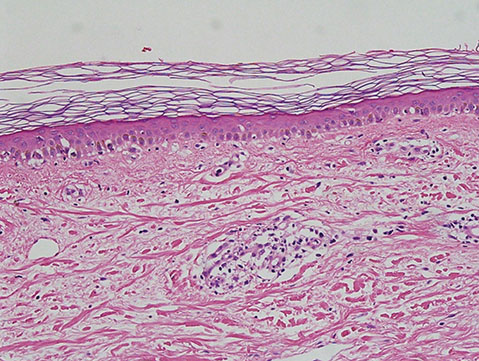
- Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome-also known as drug-induced hypersensitivity syndrome-is an uncommon disease entity that manifests as fever, skin rash, blood cell abnormalities, lymphadenopathy, and often coagulopathy. Tigecycline is an antibiotic that is selectively used to treat complicated intra-abdominal and soft-tissue infections. Recently, a few cases of tigecycline-induced coagulopathy have been reported. Herein, we report a case of tigecycline-induced coagulopathy in a patient with DRESS syndrome. Both prothrombin time and activated partial thromboplastin time were abruptly exceeded beyond 180 seconds on day 6 of tigecycline treatment and normalized after discontinuation of tigecycline.
Keyword
MeSH Terms
Figure
Reference
-
1. Cacoub P, Musette P, Descamps V, Meyer O, Speirs C, Finzi L, et al. The DRESS syndrome: a literature review. Am J Med. 2011; 124:588–597.
Article2. Kimmoun A, Dubois E, Perez P, Barbaud A, Levy B. Shock state: an unrecognized and underestimated presentation of drug reaction with eosinophilia and systemic symptoms. Shock. 2013; 40:387–391.3. Pieringer H, Schmekal B, Biesenbach G, Pohanka E. Severe coagulation disorder with hypofibrinogenemia associated with the use of tigecycline. Ann Hematol. 2010; 89:1063–1064.
Article4. Sabanis N, Paschou E, Gavriilaki E, Kalaitzoglou A, Vasileiou S. Hypofibrinogenemia induced by tigecycline: a potentially life-threatening coagulation disorder. Infect Dis (Lond). 2015; 47:743–746.
Article5. Rossitto G, Piano S, Rosi S, Simioni P, Angeli P. Life-threatening coagulopathy and hypofibrinogenaemia induced by tigecycline in a patient with advanced liver cirrhosis. Eur J Gastroenterol Hepatol. 2014; 26:681–684.
Article6. Zhang Q, Zhou S, Zhou J. Tigecycline treatment causes a decrease in fibrinogen levels. Antimicrob Agents Chemother. 2015; 59:1650–1655.
Article7. Kardaun SH, Sidoroff A, Valeyrie-Allanore L, Halevy S, Davidovici BB, Mockenhaupt M, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2007; 156:609–611.
Article8. Richard MA, Fiszenson F, Jreissati M, Jean Pastor MJ, Grob JJ. Cutaneous adverse effects during selective serotonin reuptake inhibitors therapy: 2 cases. Ann Dermatol Venereol. 2001; 128:759–761.9. Heymann WR. Addressing the role of human herpesviruses 6 and 7 in DRESS. Skinmed. 2014; 12:100–101.10. Morito H, Ogawa K, Fukumoto T, Kobayashi N, Morii T, Kasai T, et al. Increased ratio of FoxP3+ regulatory T cells/CD3+ T cells in skin lesions in drug-induced hypersensitivity syndrome/drug rash with eosinophilia and systemic symptoms. Clin Exp Dermatol. 2014; 39:284–291.
Article11. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: part I. Clinical perspectives. J Am Acad Dermatol. 2013; 68:693.12. Walsh SA, Creamer D. Drug reaction with eosinophilia and systemic symptoms (DRESS): a clinical update and review of current thinking. Clin Exp Dermatol. 2011; 36:6–11.
Article13. Bocquet H, Bagot M, Roujeau JC. Drug-induced pseudolymphoma and drug hypersensitivity syndrome (Drug Rash with Eosinophilia and Systemic Symptoms: DRESS). Semin Cutan Med Surg. 1996; 15:250–257.
Article14. Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study. Lancet Infect Dis. 2010; 10:597–602.
Article15. Barberan J, Mensa J, Farinas C, Llinares P, Olaechea P, Palomar M, et al. Recommendations of antimicrobial treatment in patients allergic to beta-lactam antibiotics. Rev Esp Quimioter. 2008; 21:60–82.16. Bergallo C, Jasovich A, Teglia O, Oliva ME, Lentnek A, de Wouters L, et al. Safety and efficacy of intravenous tigecycline in treatment of community-acquired pneumonia: results from a double-blind randomized phase 3 comparison study with levofloxacin. Diagn Microbiol Infect Dis. 2009; 63:52–61.
Article17. Morito H, Ogawa K, Kobayashi N, Fukumoto T, Asada H. Drug-induced hypersensitivity syndrome followed by persistent arthritis. J Dermatol. 2012; 39:178–179.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Drug Reaction with Eosinophilia and Systemic Symptom Syndrome Due to Everolimus: A Case Report
- Rasagiline Induced Drug Rash with Eosinophilia and Systemic Symptoms Syndrome: A Case Report
- A Case of the Drug Reaction with Eosinophilia and Systemic Symptom (DRESS) Following Isoniazid Treatment
- Drug Reaction with Eosinophilia and Systemic Symptom Syndrome Induced by Lamotrigine
- Drug reaction with eosinophilia and systemic symptom induced in a 9-year-old boy