J Korean Ophthalmol Soc.
2013 Nov;54(11):1772-1777. 10.3341/jkos.2013.54.11.1772.
Clinical Features for Patients Presenting with Diplopia
- Affiliations
-
- 1Department of Ophthalmology, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. jinchoi@paik.ac.kr
- KMID: 2217926
- DOI: http://doi.org/10.3341/jkos.2013.54.11.1772
Abstract
- PURPOSE
To evaluate the clinical features, causes and outcomes of patients with diplopia.
METHODS
All patients presenting with diplopia from October 2010 to March 2012 and followed up for more than 3 months were retrospectively investigated.
RESULTS
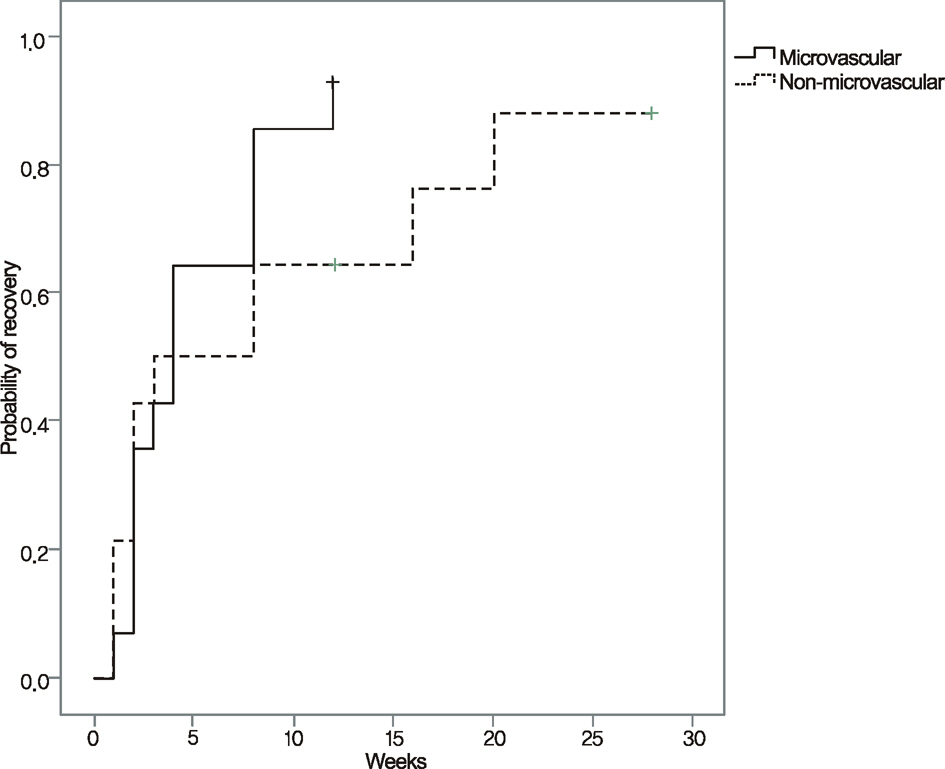
During the study period, 59 patients with diplopia were identified. There were 42 males and 17 females with an average age of 50 years. Binocular diplopia accounted for 54 cases (92%) and 5 cases (8%) had monocular diplopia. Cranial nerve palsies were the most common cause of binocular diplopia (28 cases, 52%). Within the cranial nerve palsies group, 14 cases (50%) were accompanied by hypertension or diabetes mellitus. Binocular diplopia spontaneously resolved in 35 cases (65%) by 3 months rising to 41 cases (76%) by 7 months. Thirteen (93%) out of 14 cases of cranial nerve palsies with hypertension or diabetes resolved spontaneously by 3 months.
CONCLUSIONS
Binocular diplopia was caused most commonly by cranial nerve palsy and resolved after 3 months in 65% of patients. A spontaneous recovery from diplopia was observed after 3 months in 93% of patients with cranial nerve palsies and microvascular disease such as hypertension or diabetes. Therefore, the initial observation without additional treatment would be sufficient in these patients.
MeSH Terms
Figure
Reference
-
References
1. Morris RJ. Double vision as a presenting symptom in an oph- thalmic casualty department. Eye (Lond). 1991; 5:124–9.2. Rucker JC, Tomsak RL. Binocular diplopia. A practical approach. Neurologist. 2005; 11:98–110.3. Nolan J. Diplopia. Br J Ophthalmol. 1968; 52:166–71.
Article4. Kang HJ, Ha MS. A clinical feature of the patients of orbital wall fracture with diplopia. J Korean Ophthalmol Soc. 2009; 50:969–75.
Article5. Rush JA. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol. 1992; 114:777–8.
Article6. Holmes JM, Mutyala S, Maus TL, et al. Pediatric third, fourth, and sixth nerve palsies: a population-based study. Am J Ophthalmol. 1999; 127:388–92.
Article7. Trimble R. Diplopia as a presenting sign of neoplasia. Trans Ophthalmol Soc U K. 1980; 100:498–500.8. Comer RM, Dawson E, Plant G, et al. Causes and outcomes for pa- tients presenting with diplopia to an eye casualty department. Eye (Lond). 2007; 21:413–8.9. Lepore FE, Yarian DL. Monocular diplopia of retinal origin. J Clin Neuroophthalmol. 1986; 6:181–3.10. Rush JA, Younge BR. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1,000 cases. Arch Ophthalmol. 1981; 99:76–9.11. Jacobson DM, McCanna TD, Layde PM. Risk factors for ischemic ocular motor nerve palsies. Arch Ophthalmol. 1994; 112:961–6.
Article12. Patel SV, Holmes JM, Hodge DO, Burke JP. Diabetes and hyper- tension in isolated sixth nerve palsy: a population-based study. Ophthalmology. 2005; 112:760–3.13. Prasad S, Volpe NJ. Paralytic strabismus: third, fourth, and sixth nerve palsy. Neurol Clin. 2010; 28:803–33.
Article14. Straussberg R, Cohen AH, Amir J, Varsano I. Benign abducens pal- sy associated with EBV infection. J Pediatr Ophthalmol Strabismus. 1993; 30:60.15. Shin H, Park SE. A clinical study of acquired paralytic strabismus in a secondary hospital. J Korean Ophthalmol Soc. 2007; 48:311–4.16. Park UC, Kim SJ, Hwang JM, Yu YS. Clinical features and natural history of acquired third, fourth, and sixth cranial nerve palsy. Eye (Lond). 2008; 22:691–6.
Article17. Kim HS, Lee JB, Han SH. Nontraumatic aquired paralytic strabismus. J Korean Ophthalmol Soc. 1994; 35:1127–31.18. Kim SS, Jin KH, Kim SM. Neuro-ophthalmologic evaluation of the third, fourth and sixth cranial nerve paralysis. J Korean Ophthalmol Soc. 1991; 32:283–8.19. Lee WY, Kim JH, Shin H. A clinical study of paralytic strabismus. J Korean Ophthalmol Soc. 1993; 34:549–54.20. Cackett P, Weir C, Houston CA. Transient monocular diplopia re- sulting from the treatment of amblyopia. J Pediatr Ophthalmol Strabismus. 2003; 40:245–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Immunoglobulin G4 Related Ophthalmic Disease Presenting as Diplopia and Headache
- A Case of Wegener's Granulomatosis Presenting as a Diplopia
- Orbital Myositis of the Superior Rectus Muscle Presenting as Vertical Diplopia
- Three Cases of Binocular Dipolpia Presenting after Cataract Surgery
- A Clinical Feature of the Patients of Orbital Wall Fracture With Diplopia