J Korean Ophthalmol Soc.
2013 Mar;54(3):391-395. 10.3341/jkos.2013.54.3.391.
Clinical Features of Orbital Cellulitis in Children
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University School of Medicine, Busan, Korea. hychoi@pusan.ac.kr
- KMID: 2216756
- DOI: http://doi.org/10.3341/jkos.2013.54.3.391
Abstract
- PURPOSE
The present study reviews the clinical features of orbital cellulitis in childhood for early diagnosis and proper treatment.
METHODS
The authors performed a retrospective study by computed tomography (CT) on children under 14 years of age diagnosed with orbital cellulitis and admitted to Pusan National University Hospital from 2003 to 2010.
RESULTS
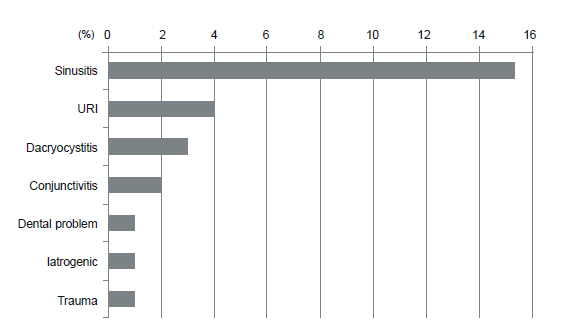
In total, 27 patients were identified (range 4 months to 14 years). Periorbital swelling was the most common initiating symptom, followed by fever and conjunctival injection. Paranasal sinus disease was the most common predisposing factor. Preseptal cellulitis was the most common finding, followed by subperiosteal abscess, orbital cellulitis, and orbital abscess. All patients underwent a blood culture; none were positive. Intravenous antibiotics therapy was performed empirically and was effective in all cases. No patients suffered from permanent complications except recurrence.
CONCLUSIONS
Orbital cellulitis in children presents with periorbital swelling, fever, conjunctival injection in association with sinusitis, and upper respiratory infection (URI). A CT study is a reliable diagnostic option for the early detection and localization in the pediatric orbital cellulitis. Early empirical antibiotic therapy is mandatory for successful treatment.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Jain A, Rubin PA. Orbital cellulitis in children. Int Ophthalmol Clin. 2001; 41:71–86.
Article2. Fearon B, Edmonds B, Bird R. Orbital-facial complications of sinusitis in children. Laryngoscope. 1979; 89:947–53.
Article3. Jackson K, Baker SR. Clinical implications of orbital cellulitis. Laryngoscope. 1986; 96:568–74.
Article4. Ferguson MP, McNab AA. Current treatment and outcome in orbital cellulitis. Aust N Z J Ophthalmol. 1999; 27:375–9.5. Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970; 80:1414–28.
Article6. Givner LB. Periorbital versus orbital cellulitis. Pediatr Infect Dis J. 2002; 21:1157–8.
Article7. Smith AT, Spencer JT. Orbital complications resulting from lesions of the sinuses. Ann Otol Rhinol Laryngol. 1948; 57:5–27.8. Jakobiec FA, Bilyk JR, Font RL. Orbit. In : Spencer WH, editor. Ophthalmic Pathology. 4th ed.Philadelphia: WB Saunders;v. 4. 1990;2861-72.9. Uzcátegui N, Warman R, Smith A, Howard CW. Clinical practice guidelines for the management of orbital cellulitis. J Pediatr Ophthalmol Strabismus. 1998; 35:73–9.
Article10. Schramm VL Jr., Curtin HD, Kennerdell JS. Evaluation of orbital cellulitis and results of treatment. Laryngoscope. 1982; 92:732–8.
Article11. Davis JP, Stearns MP. Orbital complications of sinusitis: avoid delays in diagnosis. Postgrad Med J. 1994; 70:108–10.
Article12. Liu IT, Kao SC, Wang AG, et al. Preseptal and Orbital Cellulitis: a 10-year review of hospitalized patients. J Chin Med Assoc. 2006; 69:415–22.
Article13. Brown CL, Graham SM, Griffin MC, et al. Pediatric medial sub-394 www.ophthalmology.orgperiosteal orbital abscess: medical management where possible. Am J Rhinol. 2004; 18:321–7.14. Barone SR, Aiuto LT. Periorbital and orbital cellulitis in the Haemophilus influenzae vaccine era. J Pediatr Ophthalmol Strabismus. 1997; 34:293–6.
Article15. Ambati BK, Ambati J, Azar N, et al. Periorbital and orbital cellulitis before and after the advent of Haemophilus influenzae type B vaccination. Ophthalmology. 2000; 107:1450–3.
Article16. Donahue SP, Schwartz G. Preseptal and orbital cellulitis in childhood. A changing microbiologic spectrum. Ophthalmology. 1998; 105:1902–5.
Article17. Watters EC, Wallar PH, Hiles DA, Michaels RH. Acute orbital cellulitis. Arch Ophthalmol. 1976; 94:785–8.
Article18. Schwartz GR, Wright SW. Changing bacteriology of periorbital cellulitis. Ann Emerg Med. 1996; 28:617–20.
Article19. Zimmerman RK. Pneumococcal conjugate vaccine for young children. Am Fam Physician. 2001; 63:1991–8.20. Chang CH, Lai YH, Wang HZ, et al. Antibiotic treatment of orbital cellulitis: an analysis of pathogenic bacteria and bacterial susceptibility. J Ocul Pharmacol Ther. 2000; 16:75–9.
Article21. Sadow KB, Chamberlain JM. Blood cultures in the evaluation of children with cellulitis. Pediatrics. 1998; 101:E4.
Article22. Teele DW. Management of the child with a red and swollen eye. Pediatr Infect Dis. 1983; 2:258–62.23. Rahbar R, Robson CD, Petersen RA, et al. Management of orbital subperiosteal abscess in children. Arch Otolaryngol Head Neck Surg. 2001; 127:281–6.
Article24. Wald ER. Periorbital and orbital infections. In : Long SS, Pickering LK, Prober CG, editors. Principles and Practice of Pediatric Infectious Diseases. 2nd ed.New York: NY Churchill Livingstone;2003. p. 508–13.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Retinoblastoma Manifested by Hyphema and Orbital Cellulitis
- Orbital and Periorbital Cellulitis in Children: A Recent 7-Year Clinical Rev iew
- Clinical Characteristics of Orbital Cellulitis in Children
- A Case ef Orbital Cellulitis Subdural Subdural Abscess
- Clinical Review of Orbital Complications Caused by Paranasal Sinusitis: 10-Years Experience