J Korean Ophthalmol Soc.
2011 Dec;52(12):1461-1469. 10.3341/jkos.2011.52.12.1461.
Bleb Morphology of Fornix-Based Versus Limbus-Based Conjunctival Flaps in Trabeculectomy with Mitomycin C
- Affiliations
-
- 1Cheil Eye Hospital, Daegu, Korea. eye7575@korea.com
- KMID: 2215150
- DOI: http://doi.org/10.3341/jkos.2011.52.12.1461
Abstract
- PURPOSE
To compare the bleb morphology and surgical outcomes of a limbus-based group with those of a fornix-based group who underwent trabeculectomy with mitomycin C (MMC).
METHODS
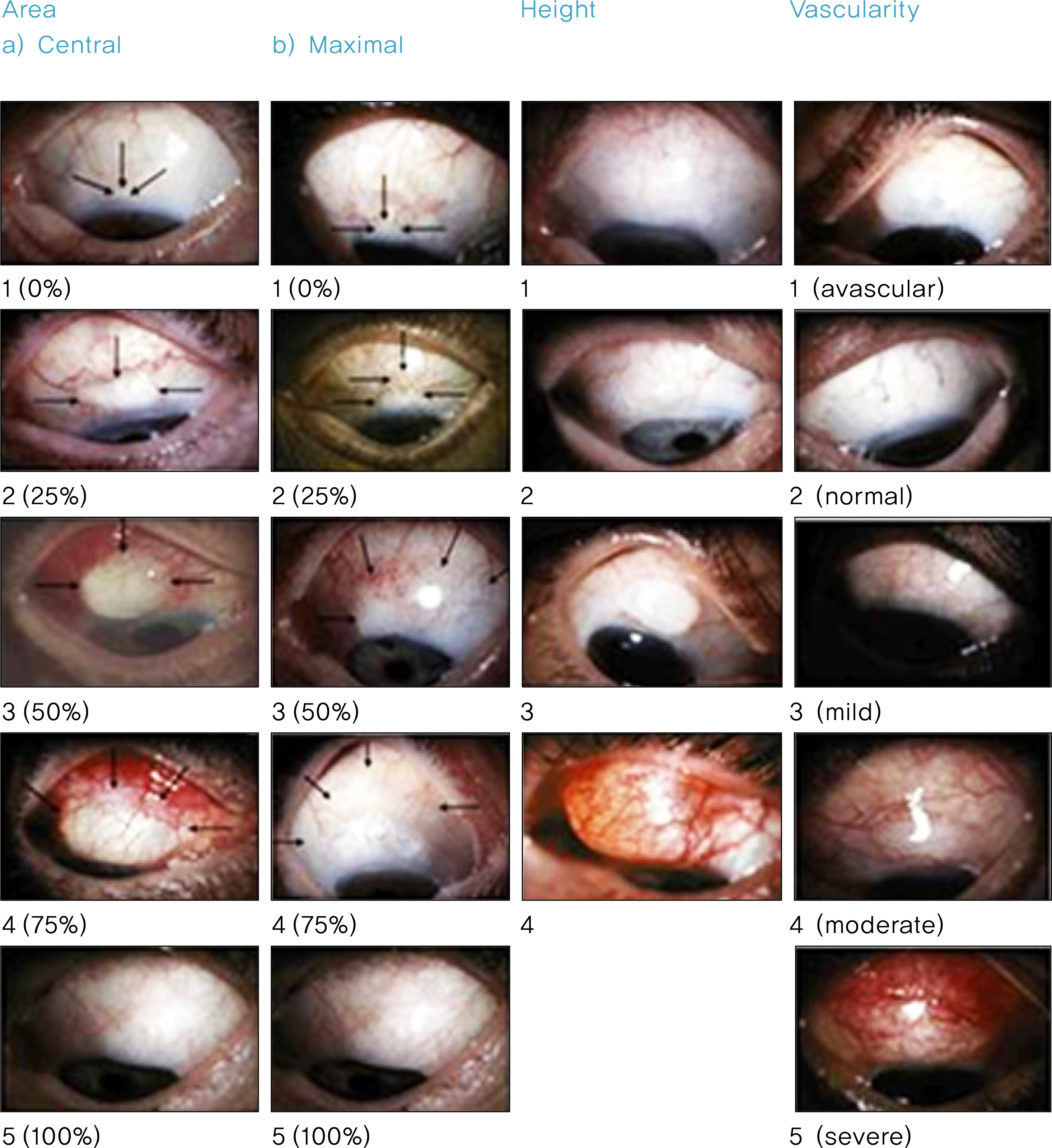
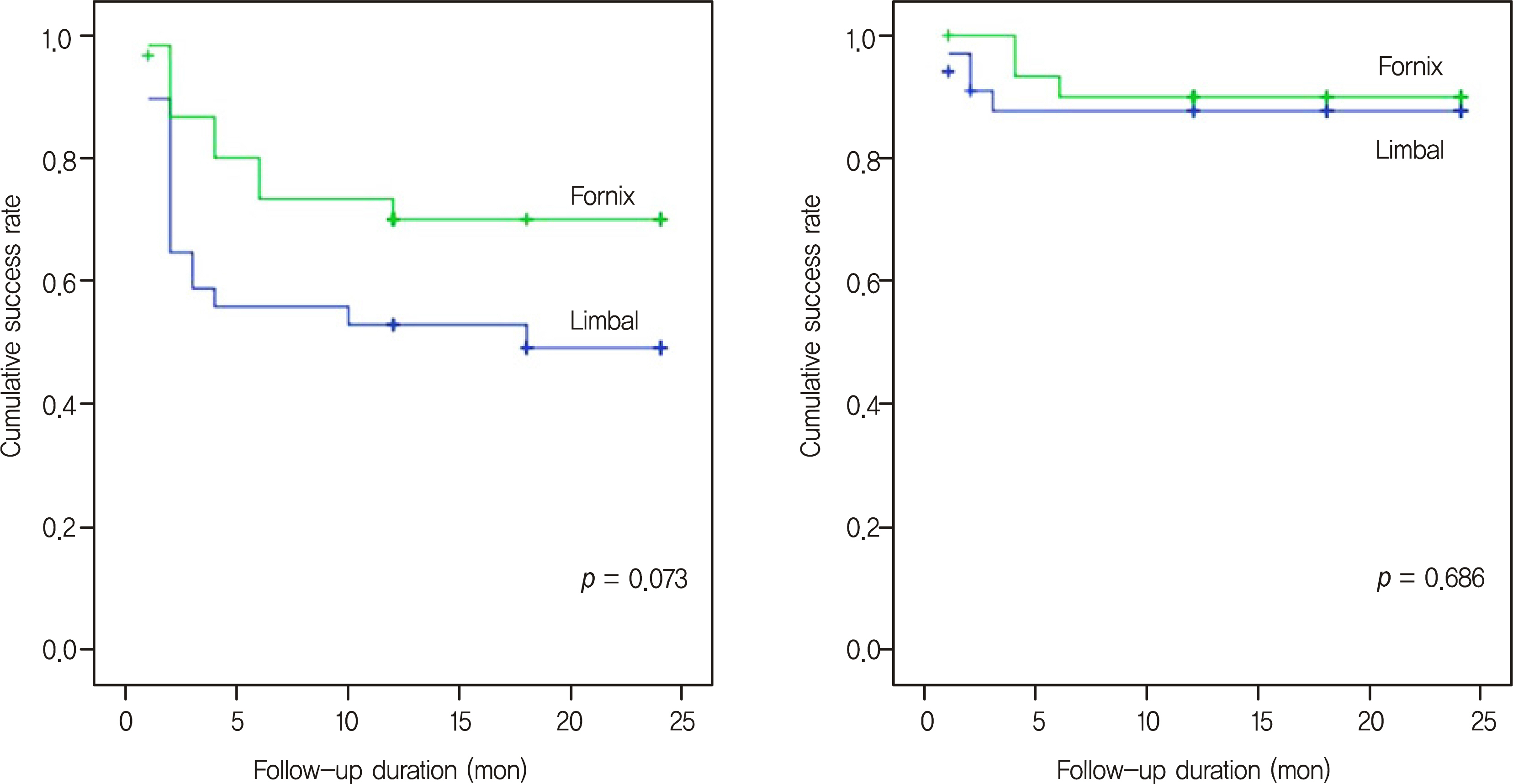
Sixty-five eyes of 59 patients who had undergone trabeculectomy with MMC and who were observed for one year or more were included in the present study. A limbus-based conjunctival flap was used for 34 eyes of 31 patients and a fornix-based conjunctival flap for the other 31 eyes of 28 patients. The bleb morphologies were classified and compared after one year or more postoperatively according to the Moorfield Bleb Grading System, and intraocular pressure and success rates were evaluated.
RESULTS
The central bleb vascularity of the limbus-based group was statistically significantly lower than that of the fornix- based group (1.79 +/- 0.64; 2.16 +/- 0.73, p = 0.042). The risk of cystic bleb formation was higher in the limbus-based group (38.2%; 16.5%, p = 0.047). There were no differences in the IOP or success rate between the two groups.
CONCLUSIONS
There were no differences between the two groups with regard to the IOP or cumulative success rate. However, in the fornix-based group, the central bleb vascularity was lower and the risk of avascular cystic bleb formation was higher than those in the limbus-based group.
Keyword
Figure
Reference
-
References
1. Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol. 1968; 66:673–9.2. Picht G, Grehn F. Classification of filtering blebs in trabeculectomy: biomicroscopy and functionality. Curr Opin Ophthalmol. 1998; 9:2–8.
Article3. Soltau JB, Rothman RF, Budenz DL, et al. Risk factors for glaucoma filtering bleb infections. Arch Ophthalmol. 2000; 118:338–42.
Article4. Watson PG. Surgery of the glaucomas. Br J Ophthalmol. 1972; 56:299–306.
Article5. Sanders R, MacEwen CJ, Haining WM. Trabeculectomy: effect of varying the surgical site. Eye. 1993; 7:440–3.6. Negi AK, Kiel AW, Vernon SA. Does the site of filtration influence the medium to long term intraocular pressure control following mi-crotrabeculectomy in low risk eyes? Br J Ophthalmol. 2004; 88:1008–11.
Article7. Kronfeld FC. The chemical demonstration of transconjunctival passage of aqueous after antiglaucomatous operations. Am J Ophthalmol. 1952; 35:38–45.
Article8. Cantor LB, Mantravadi A, WuDunn D, et al. Morphologic classification of filtering blebs after glaucoma filtration surgery: the Indiana Bleb Appearance Grading Scale. J Glaucoma. 2003; 12:266–71.
Article9. Wells AP, Crowston JG, Marks J, et al. A pilot study of system for grading of drainage blebs after glaucoma surgery. J Glaucoma. 2004; 13:454–60.10. Yamamoto T, Sakuma T, Kitazawa Y. An ultrasound biomicro-scopic study of filtering blebs after mitomycin C trabeculectomy. Ophthalmology. 1995; 102:1770–6.11. Pavlin CJ, Harasiewicz K, Foster FS. Ultrasound biomicroscopy of anterior segment structures in normal and glaucomatous eyes. Am J Ophthalmol. 1992; 113:381–9.
Article12. Shin JY, Kang SY, Kim NR, et al. The morphometric analysis of filtering bleb using anterior segment optical coherence tomography: pilot study. J Korean Ophthalmol Soc. 2010; 51:234–40.
Article13. Wells AP, Ashraff NN, Hall RC, Purdie G. Comparison of two clinical bleb grading systems. Ophthalmology. 2006; 113:77–83.
Article14. el Sayyad F, el-Rashood A, Helal M, et al. Fornix-based versus lim-bal-based conjunctival flaps in initial trabeculectomy with postoperative 5-fluorouracil: four-year followup findings. J Glaucoma. 1999; 8:124–8.15. Alwitry A, Patel V, King AW. Fornix vs limbal-based trabeculectomy with mitomycin C. Eye. 2005; 19:631–6.
Article16. Traverso CE, Tomey KF, Antonios S. Limbal- vs fornix-based conjunctival trabeculectomy flaps. Am J Ophthalmol. 1987; 104:28–32.
Article17. Shuster JN, Krupin T, Kolker AE, Becker B. Limbus- v for-nix-based conjunctival flap in trabeculectomy. A long-term randomized study. Arch Ophthalmol. 1984; 102:361–2.18. Brincker P, Kessing SV. Limbus-based versus fornix-based conjunctival flap in glaucoma filtering surgery. Acta Ophthalmol (Copenh). 1992; 70:641–4.
Article19. Wells AP, Cordeiro MF, Bunce C, Khaw PT. Cystic bleb formation and related complications in limbus- versus fornix-based conjunctival flaps in pediatric and young adult trabeculectomy with mitomycin C. Ophthalmology. 2003; 110:2192–7.
Article20. Agbeja AM, Dutton GN. Conjunctival incisions for trabeculectomy and their relationship to the type of bleb formation - a pre-liminary study. Eye. 1987; 1:738–43.21. Wee WR, Youn DH. Trabeculectomy using a fornix-based conjunctival flap. J Korean Ophthalmol Soc. 1986; 27:819–22.22. Boo SD, Jun SY, Hong YJ. A clinical comparision of the effect of limbal-based vs fornix-based conjunctival flaps in trabeculectomy. J Korean Ophthalmol Soc. 1990; 31:1439–44.23. Shin IH, Hyung SM. Outcome of fornix-based versus limbal-based conjunctival flaps in trabeculectomy with mitomycin C. J Korean Ophthalmol Soc. 2003; 44:2829–37.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcome of Fornix-Based Versus Limbus-Based Conjunctival Flaps in Trabeculectomy with Mitomycin C
- Trabeculectomy Using a Fornix-based Conjunctival Flap
- A suture technique for the management of conjunctival wound leakage
- Change of Conjunctival Sensitivity after Trabeculectomy
- Conjunctival impression cytology of the filtering bleb