J Korean Ophthalmol Soc.
2015 Oct;56(10):1572-1579. 10.3341/jkos.2015.56.10.1572.
Clinical Outcomes of Minimal Exposure to Indocyanine Green-Assisted Peeling of the Internal Limiting Membrane
- Affiliations
-
- 1Hangil Eye Hospital, Incheon, Korea. Parkys73@lycos.co.kr
- KMID: 2214417
- DOI: http://doi.org/10.3341/jkos.2015.56.10.1572
Abstract
- PURPOSE
To evaluate the clinical outcomes of epiretinal membrane (ERM) surgery with minimal exposure to indocyanine green (ICG) dye-assisted internal limiting membrane (ILM) peeling compared with no ICG dye.
METHODS
We divided 33 eyes with ERM treated by vitrectomy into 2 groups. ICG dye was used in the first group of 18 eyes (ICG group) but not in the second group of 15 eyes (no dye [ND] group). In the ICG group, 0.25% diluted ICG dye was injected into the fluid-filled eye and removed with a back-flushing needle after 3-5 seconds to peel ILM. Value changes in several parameters including visual acuity, central macular thickness, Humphrey automated kinetic perimetric analysis, and peripapillary retinal nerve fiber layer (RNFL) thickness were followed up and compared according to ICG dye use.
RESULTS
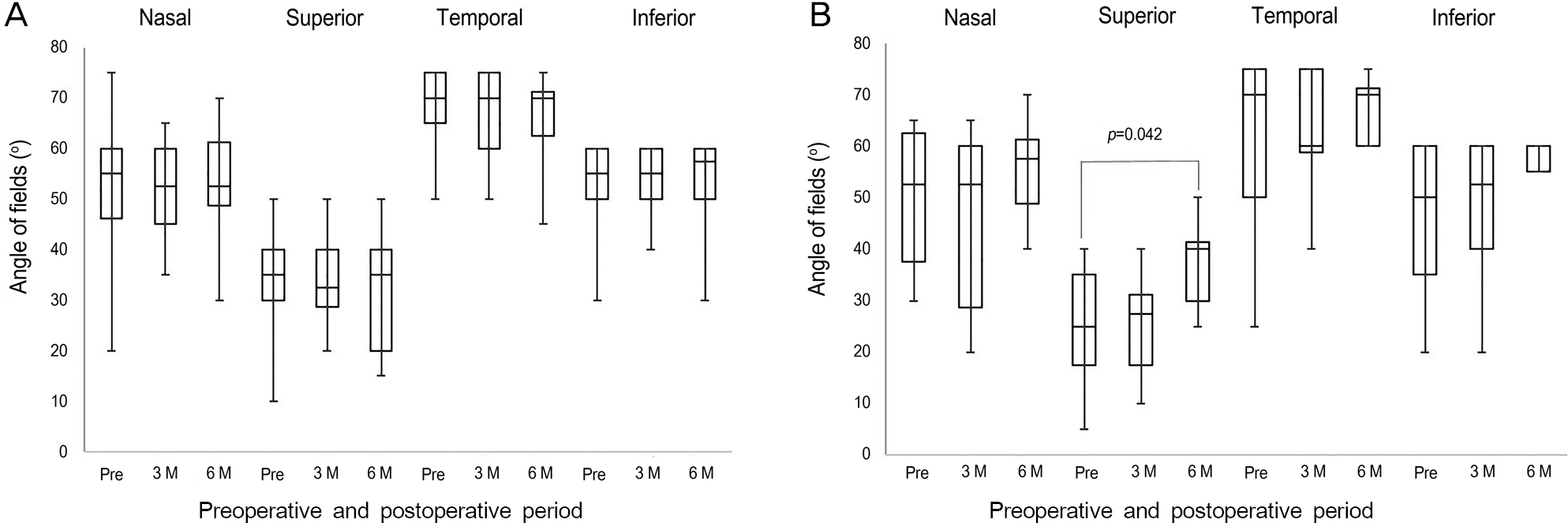
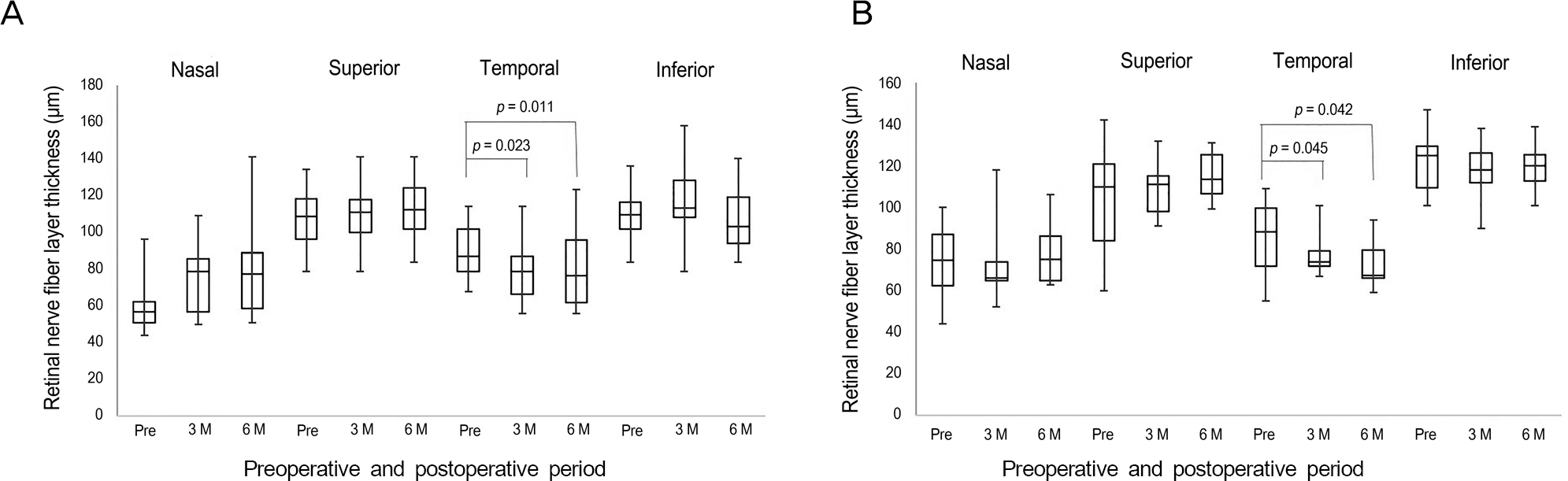
No differences were found between the 2 groups in terms of visual acuity, central macular thickness, and peripapillary RNFL thickness preoperatively and at 6 months postoperatively (p = 0.125 for visual acuity, p = 0.734 for central macular thickness, p = 0.615 for RNFL thickness). Six months after surgery, no significant increase was found in any region of visual field in the ICG group (p = 0.392). The visual field was significantly increased in the superior region in the ND group (p = 0.042). The RNFL thickness in the temporal quadrant was significantly reduced at 6 months postoperatively compared to baseline values in both groups (p = 0.011 for ICG group, p = 0.042 for ND group).
CONCLUSIONS
ICG dye-assisted ILM peeling does not aggravate clinical outcomes of ERM surgery in terms of visual acuity, central macular thickness, visual fields, or RNFL thickness and can be safely utilized with proper techniques.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Klein R, Klein BE, Wang Q, Moss SE. The epidemiology of epi-retinal membranes. Trans Am Ophthalmol Soc. 1994; 92:403–25. discussion 425-30.2. de Bustros S, Thompson JT, Michels RG. . Vitrectomy for idio-pathic epiretinal membranes causing macular pucker. Br J Ophthalmol. 1988; 72:692–5.
Article3. Machemer R. The surgical removal of epiretinal macular mem-branes (macular puckers). Klin Monbl Augenheilkd. 1978; 173:36–42.4. Grewing R, Mester U. Results of surgery for epiretinal membranes and their recurrences. Br J Ophthalmol. 1996; 80:323–6.
Article5. Shimada H, Nakashizuka H, Hattori T. . Double staining with brilliant blue G and double peeling for epiretinal membranes. Ophthalmology. 2009; 116:1370–6.
Article6. Lee JE, Yoon TJ, Oum BS. . Toxicity of indocyanine green in-jected into the subretinal space: subretinal toxicity of indocyanine green. Retina. 2003; 23:675–81.7. Da Mata AP, Burk SE, Riemann CD. . Indocyanine green-as-sisted peeling of the retinal internal limiting membrane during vi-trectomy surgery for macular hole repair. Ophthalmology. 2001; 108:1187–92.
Article8. Ando F, Sasano K, Ohba N. . Anatomic and visual outcomes after indocyanine green-assisted peeling of the retinal internal lim-iting membrane in idiopathic macular hole surgery. Am J Ophthalmol. 2004; 137:609–14.
Article9. Gass CA, Haritoglou C, Schaumberger M, Kampik A. Functional outcome of macular hole surgery with and without indocyanine green-assisted peeling of the internal limiting membrane. Graefes Arch Clin Exp Ophthalmol. 2003; 241:716–20.
Article10. Uemura A, Kanda S, Sakamoto Y, Kita H. Visual field defects after uneventful vitrectomy for epiretinal membrane with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol. 2003; 136:252–7.
Article11. Kanda S, Uemura A, Yamashita T. . Visual field defects after intravitreous administration of indocyanine green in macular hole surgery. Arch Ophthalmol. 2004; 122:1447–51.12. Nagai N, Ishida S, Shinoda K. . Surgical effects and complica-tions of indocyanine green-assisted internal limiting membrane peeling for idiopathic macular hole. Acta Ophthalmol Scand. 2007; 85:883–9.
Article13. Sekiryu T, Iida T. Long-term observation of fundus infrared fluo-rescence after indocyanine green-assisted vitrectomy. Retina. 2007; 27:190–7.
Article14. von Jagow B, Höing A, Gandorfer A. . Functional outcome of indocyanine green-assisted macular surgery: 7-year follow-up. Retina. 2009; 29:1249–56.15. Gandorfer A, Haritoglou C, Gass CA. . Indocyanine green-as-sisted peeling of the internal limiting membrane may cause retinal damage. Am J Ophthalmol. 2001; 132:431–3.
Article16. Yam HF, Kwok AK, Chan KP. . Effect of indocyanine green and illumination on gene expression in human retinal pigment epi-thelial cells. Invest Ophthalmol Vis Sci. 2003; 44:370–7.
Article17. Murata M, Shimizu S, Horiuchi S, Sato S. The effect of in-docyanine green on cultured retinal glial cells. Retina. 2005; 25:75–80.
Article18. Gandorfer A, Haritoglou C, Gandorfer A, Kampik A. Retinal dam-age from indocyanine green in experimental macular surgery. Invest Ophthalmol Vis Sci. 2003; 44:316–23.
Article19. Haritoglou C, Priglinger S, Gandorfer A. . Histology of the vit-reoretinal interface after indocyanine green staining of the ILM, with illumination using a halogen and xenon light source. Invest Ophthalmol Vis Sci. 2005; 46:1468–72.
Article20. Song BY, Ahn KY, Seo MS. Internal limiting membrane peeling using indocyanine green in vitrectomy for idiopathic macular hole. J Korean Ophthalmol Soc. 2004; 45:444–50.21. Lee JE, Oum BS. Macular hole surgery with or without in-docyanine green-assisted internal limiting membrane peeling. J Korean Ophthalmol Soc. 2003; 44:2553–9.22. Nam DH, Hwang S, Huh K. Idiopathic macular hole surgery with or without indocyanine green-stained internal limiting membrane peeling. J Korean Ophthalmol Soc. 2004; 45:1086–91.23. Hillenkamp J, Saikia P, Herrmann WA. . Surgical removal of idiopathic epiretinal membrane with or without the assistance of indocyanine green: a randomised controlled clinical trial. Graefes Arch Clin Exp Ophthalmol. 2007; 245:973–9.
Article24. Wu Y, Zhu W, Xu D. . Indocyanine green-assisted internal lim-iting membrane peeling in macular hole surgery: a meta-analysis. PLoS One. 2012; 7:e48405.
Article25. Schmid-Kubista KE, Lamar PD, Schenk A. . Comparison of macular function and visual fields after membrane blue or in-fracyanine green staining in vitreoretinal surgery. Graefes Arch Clin Exp Ophthalmol. 2010; 248:381–8.
Article26. Lee SB, Shin YI, Jo YJ, Kim JY. Longitudinal changes in retinal nerve fiber layer thickness after vitrectomy for epiretinal membrane. Invest Ophthalmol Vis Sci. 2014; 55:6607–11.
Article27. Kim CY, Lee JH, Lee SJ. . Visual field defect caused by nerve fiber layer damage associated with an internal limiting lamina de-fect after uneventful epiretinal membrane surgery. Am J Ophthalmol. 2002; 133:569–71.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Outcomes of ILM Peeling Using Triamcinolone and Indocyanine Green during Idiopathic Macular Hole Surgery
- Clinical Outcomes of Indocyanine Green-Assisted Peeling of the Internal Limiting Membrane in Epiretinal Membrane Surgery
- Macular Hole Surgery with or without Indocyanine Green-Assisted Internal Limiting Membrane Peeling
- Idiopathic Macular Hole Surgery with or without Indocyanine Green-Stained Internal Limiting Membrane Peeling
- The Outcomes After Indocyanine Green-assisted Peeling of the Internal Limiting Membrane in Macular Hole Surgery