J Korean Surg Soc.
2013 Dec;85(6):261-268. 10.4174/jkss.2013.85.6.261.
Variation or newly identified glissonian pedicles between the lateral and medial sections of the liver, using cadaver dissection
- Affiliations
-
- 1Department of Surgery, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- 2Department of Surgery, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea. wanghj@ajou.ac.kr
- KMID: 2212547
- DOI: http://doi.org/10.4174/jkss.2013.85.6.261
Abstract
- PURPOSE
Studies of liver anatomy have developed alongside clinical achievements, as these types of research complement each other. The aim of this study is to determine whether or not the portal vein branches (P4d) in 'Nagino's trisectionectomy' exist, and to examine their characteristics using cadaver dissection.
METHODS
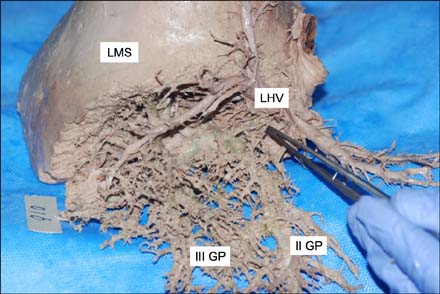
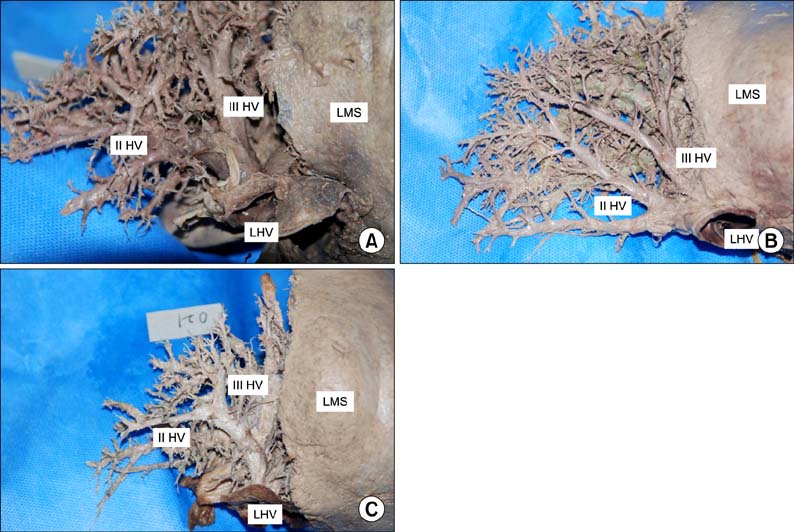
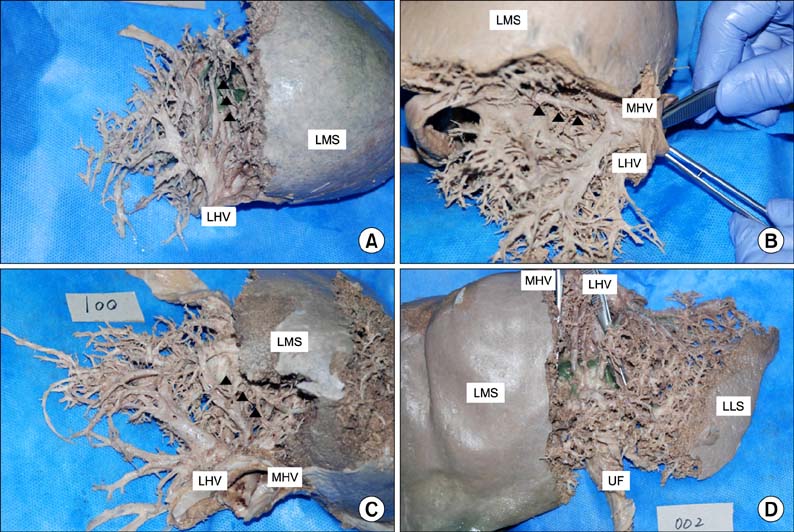
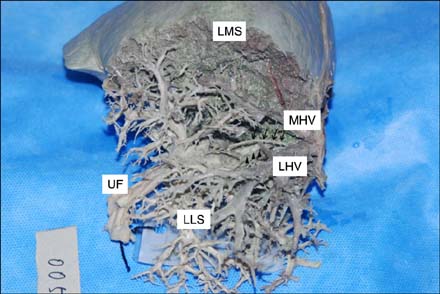
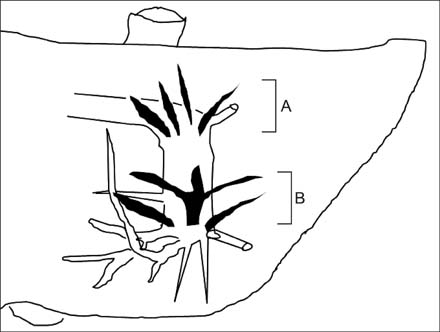
From April 2012 to July 2012, 31 adult cadavers were delicately dissected. We defined a 'NewGP' as an extra glissonian pedicle (GP) other than the traditional GPs that supply segments II, III, IVa, and IVb in the ordinary direction, and anatomically located superior to the umbilical fissure (UF).
RESULTS
We identified 'NewGPs' based on the UF and UF vein. The incidence of 'NewGPs' was 30/31 (96.8%). The diameter of the 'NewGPs' ranged from 3.5 to 5.6 mm, which was not significantly different from that of traditional GPs (II-, III-, or IV-GP), which have diameters ranging from 3.7 to 9.7 mm.
CONCLUSION
We think that the P4d in 'Nagino's trisectionectomy' correspond to the 'IVa NewGP' and the additional pedicle. We believe the clinical significance of the 'NewGP' is to complement the traditional II, III, IVa, and IVb pedicles in supplying the liver.
Keyword
MeSH Terms
Figure
Reference
-
1. Couinaud C. Controlled hepatectomies and exposure of the intrahepatic bile ducts: anatomical and technical study. Paris: C. Couinaud;1981.2. Healey JE Jr, Schroy PC. Anatomy of the biliary ducts within the human liver; analysis of the prevailing pattern of branchings and the major variations of the biliary ducts. AMA Arch Surg. 1953; 66:599–616.3. Ryu M, Cho A. New liver anatomy: portal segmentation and the drainage vein. New York: Springer;2009.4. Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005; 12:351–355.5. Couinaud C. Portal segmentation. In : Couinaud C, editor. Controlled hepatectomies and exposure of the intrahepatic bile ducts: anatomical and technical study. Paris: C. Couinaud;1981. p. 9–17.6. Strasberg SM. Terminology of liver anatomy and liver resections: coming to grips with hepatic Babel. J Am Coll Surg. 1997; 184:413–434.7. Botero AC, Strasberg SM. Division of the left hemiliver in man: segments, sectors, or sections. Liver Transpl Surg. 1998; 4:226–231.8. Couinaud C. Liver anatomy: portal (and suprahepatic) or biliary segmentation. Dig Surg. 1999; 16:459–467.9. Belghiti J, Guevara OA, Noun R, Saldinger PF, Kianmanesh R. Liver hanging maneuver: a safe approach to right hepatectomy without liver mobilization. J Am Coll Surg. 2001; 193:109–111.10. Sato TJ, Hirai I, Murakami G, Kanamura T, Hata F, Hirata K. An anatomical study of short hepatic veins, with special reference to delineation of the caudate lobe for hanging maneuver of the liver without the usual mobilization. J Hepatobiliary Pancreat Surg. 2002; 9:55–60.11. Hirai I, Murakami G, Kimura W, Kanamura T, Sato I. How should we treat short hepatic veins and paracaval branches in anterior hepatectomy using the hanging maneuver without mobilization of the liver? An anatomical and experimental study. Clin Anat. 2003; 16:224–232.12. Kim BW, Wang HJ, Kim WH, Kim MW. Favorable outcomes of hilar duct oriented hepatic resection for high grade Tsunoda type hepatolithiasis. World J Gastroenterol. 2006; 12:431–436.13. Kim IG, Jeon JY, Jung JP, Chon SE, Kim HJ, Kim DJ, et al. Totally laparoscopic left hemihepatectomy using ventral hilum exposure (VHE) for intrahepatic bile duct stone. J Laparoendosc Adv Surg Tech A. 2010; 20:143–146.14. Kwon D, Murakami G, Hata F, Wang HJ, Chung MS, Hirata K. Location of the ventral margin of the paracaval portion of the caudate lobe of the human liver with special reference to the configuration of hepatic portal vein branches. Clin Anat. 2002; 15:387–401.15. Kwon D, Murakami G, Wang HJ, Chung MS, Hata F, Hirata K. Ventral margin of the paracaval portion of human caudate lobe. J Hepatobiliary Pancreat Surg. 2001; 8:148–153.16. Nagino M, Kamiya J, Arai T, Nishio H, Ebata T, Nimura Y. "Anatomic" right hepatic trisectionectomy (extended right hepatectomy) with caudate lobectomy for hilar cholangiocarcinoma. Ann Surg. 2006; 243:28–32.17. Takayasu K, Moriyama N, Muramatsu Y, Shima Y, Goto H, Yamada T. Intrahepatic portal vein branches studied by percutaneous transhepatic portography. Radiology. 1985; 154:31–36.18. Launois B, Jamieson GG. Segmentectomy procedures: the leftliver. In : Launois B, Jamieson GG, editors. Modern operative techniques in liver surgery. New York: Churchill Livingstone;1993. p. 51–65.19. Reichert PR, Renz JF, D'Albuquerque LA, Rosenthal P, Lim RC, Roberts JP, et al. Surgical anatomy of the left lateral segment as applied to living-donor and split-liver transplantation: a clinicopathologic study. Ann Surg. 2000; 232:658–664.20. Hata F, Hirata K, Murakami G, Mukaiya M. Identification of segments VI and VII of the liver based on the ramification patterns of the intrahepatic portal and hepatic veins. Clin Anat. 1999; 12:229–244.21. Kim IG, Park JW, Kim BW, Wang HJ, Lee BH, Kim MW. Safety of 'isolated IVb (inferior) resection of the liver' by cadaver dissection. Korean J Hepatobiliary Pancreat Surg. 2005; 9:1–5.22. Kim IG, Park JW, Lee TH, Kim BW, Wang HJ, Kim MW. Surgical anatomy of left lobe of the liver (Couinaud's and Healey's anatomy) through Korean cadaver liver dissection. Korean J Hepatobiliary Pancreat Surg. 2005; 9:73–77.23. Hwang S, Lee SG, Choi ST, Moon DB, Ha TY, Lee YJ, et al. Hepatic vein anatomy of the medial segment for living donor liver transplantation using extended right lobe graft. Liver Transpl. 2005; 11:449–455.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety of 'Isolated IVb (Inferior) Resection of the Liver' by Cadaver Dissection
- Anatomical Variation of the Glissonean Pedicle of the Right Liver
- Uncommon configuration of intercostobrachial nerves, lateral roots, and absent medial cutaneous nerve of arm in a cadaveric study
- Anatomical variation of quadratus plantae with flexor digitorum longus tendon along with unilateral polydactyly of the toes: a rare case report
- Superficial course of the medial plantar nerve: case report