J Korean Ophthalmol Soc.
2009 Jul;50(7):1098-1104. 10.3341/jkos.2009.50.7.1098.
Effects of Medpor(R) Sheet as Substitute for Tarsus in Eyelid Reconstruction
- Affiliations
-
- 1Department of Ophthalmology, Dongkang General Hospital, Ulsan, Korea. Lavie2k@korea.com
- KMID: 2212501
- DOI: http://doi.org/10.3341/jkos.2009.50.7.1098
Abstract
- PURPOSE
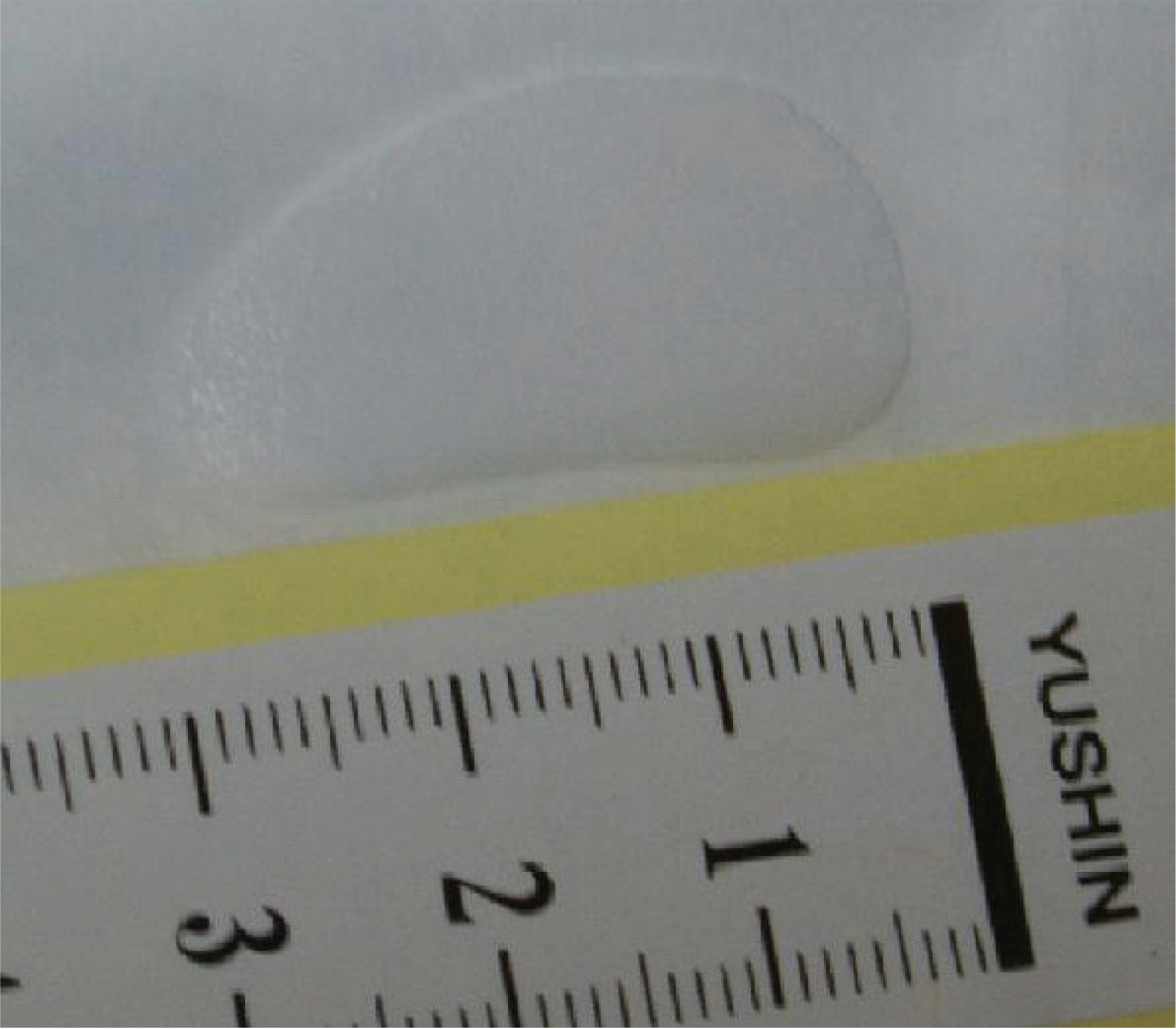
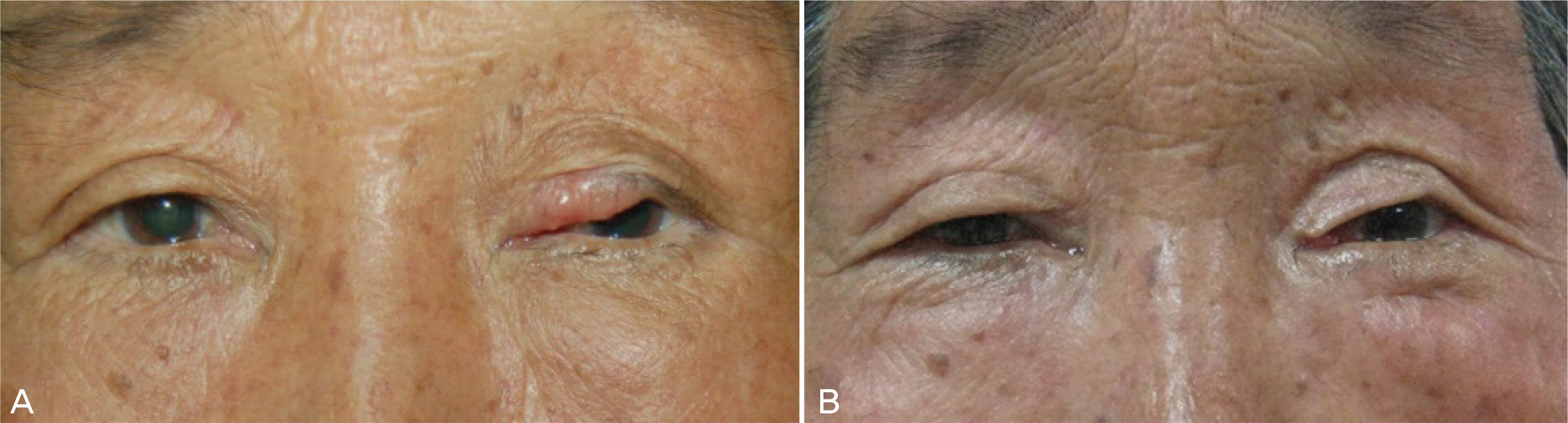
To report a simple surgical technique for rebuilding the palpebral tarsal plate using a Medpor(R) sheet. The formation of a palpebral tarsal plate is very important in the reconstruction of the eyelid. Transplantation of cartilaginous tissue is often necessary to create the palpebral tarsal plate. However obtaining enough cartilaginous tissue is difficult. CASE SUMMARY: Eyelid reconstruction and surgical resection of each lesion was attempted on two patients clinically diagnosed with basal cell carcinoma and sebaceous gland carcinoma between August, 2006 and November, 2007. Reconstruction was performed using a modified Cutler-Beard method or the sebaceous gland carcinoma that occurred in the upper eyelid, and a modified Tenzel semicircular rotational flap procedure was used or the basal cell carcinoma that occurred in the lower eyelid. For the reconstruction of tarsus, 0.45 mm Medpor(R) sheet was used. Complications, such as shortage of eyelid movement, dragging of eyelid or unstable eyelid margin, did not occur after the operations in either subject. In the case of the upper eyelid reconstruction, the eyelid became stiff at the early stage, but the condition improved after 6 months. CONCLUSIONS: The reconstruction of the palpebral tarsal plate using a Medpor(R) sheet is considered an effective and safe technique for the reconstruction of an eyelid.
Figure
Cited by 1 articles
-
The Effects of Commodified Growth Factor Products on the Fibrovascularization of Porous Polyethylene Orbital Implants
Won Mo Gu, Joon Hyuk Choi, Jun Hyuk Son
J Korean Ophthalmol Soc. 2014;55(9):1366-1371. doi: 10.3341/jkos.2014.55.9.1366.
Reference
-
References
1. Müllner K, Langmann G. Chondroplast. A new material for eyelid reconstruction. Ophthalmologica. 1999; 213:189–93.2. Holt JE, Holt GR, van Kirk M. Use of temporalis fascia in eyelid reconstruction. Ophthalmology. 1984; 91:89–93.
Article3. Shorr N, Perry JD, Goldberg RA, et al. The safety and applications of acellular human dermal allograft in ophthalmic plastic and reconstructive surgery: a preliminary report. Ophthal Plast Reconstr Surg. 2000; 16:223–30.4. Debacker CM, Dutton JJ, Proia AD, et al. A comparative study of bovine pericardium (periguard) and homologous sclera as lower eyelid spacer graft analogs in New Zealand white rabbits. Ophthal Plast Reconstr Surg. 2000; 16:156–61.
Article5. Kim YM, Son MG, Kim YD. Hard palate mucosa grafts for lower lid retraction. J Korean Ophthalmol Soc. 2000; 41:2319–26.6. Kim SD, Koh SI, Park KS, Kim JD. Surgical correction of lower lid retraction using the scleral spacer. J Korean Ophthalmol Soc. 1998; 39:3083–7.7. Fay AM, Pieroth L, Rubin PA. An animal model of lower eyelid spacer grafting with acellular dermis. Ophthal Plast Reconstr Surg. 2001; 17:270–5.
Article8. Rubin PA, Bilyk JR, Shore JW. Orbital reconstruction using porous polyethylene sheets. Ophthalmology. 1994; 101:1697–708.
Article9. Rubin PA, Popham JK, Bilyk JK, Shore JW. Comparison of fibrovascular ingrowth into hydroxyapatite and porous polyethylene orbital implants. Ophthal Plast Reconstr Surg. 1994; 10:96–103.
Article10. Bilyk JK, Rubin PA, Shore JW. Correction of enophthalmos with porous polyethylene implants. Int Ophthalmol Clin. 1992; 32:151–6.
Article11. Kwon JS, Park IK, Khwarg SI. The preventive effect of porous polyethylene sheet on the slippage of Prolene® loop placed in the subcutaneous tissue of rabbits. J Korean Ophthalmol Soc. 2003; 44:402–9.12. Im J-Y, Jang JU, Mun SH. Lid reconstruction using the porous polyethylene (Medpor®) sheet. J Korean Ophthalmol Soc. 2003; 44:2111–6.13. Karesh JW, Dresner SC. High-density porous polyethylene (Medpor) as a successful anophthalmic socket implant. Ophthalmology. 1994; 101:1688–96.
Article14. Nicaeus TE, Tolentino MJ, Adamis AP, Rubin PA. Sucralfate and basic fiboblast growth factor promote endothelial cell proliferation around porous alloplastic implants in vitro. Ophthal Plast Reconstr Surg. 1996; 12:235–9.15. Wong JF, Soparkar CN, Patrinely JR. Correction of lower eyelid retraction with high density porous polyethylene: The Medpor® lower eyelid spacer. Orbit. 2001; 20:217–25.16. O'Brien T, Cranston D, Fuggle SL. Two mechanisms of basic fibroblast growth factor-induced angiogenesis in bladder cancer. Cancer Res. 1997; 57:136–40.17. Relf M, Lejeune S, Scott PA, et al. Expression of the angiogenesis factors vascular endothelial cell growth factor, acidic and basic fibroblast growth factor, tumor growth factor β-1, platelet- derived endothelial cell growth factor, placenta growth factor, and pleiotrophin in human primary breast cancer and its relation to angiogenesis. Cancer Res. 1997; 57:963–9.18. Bigham WJ, Stanley P, Cahill JM. Fibrovascular ingrowth in porous ocular implants: The effect of material composition, poro-sity, growth factors, and coatings. Ophthal Plast Reconstr Surg. 1999; 15:317–25.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lid Reconstruction Using the Porous Polyethylene (Medpor(R)) Sheet
- Upper Eyelid Reconstruction Using the Medpor(R) Sheet and Median Forehead Flap
- Clinical Experience of Orbital wall Reconstruction using Medpor(R) Barrier Sheet Implant
- Comparative Observation of Barrier Sheet and Nonbarrier Sheet Medpor(R) Inserted on Orbital Floor in Rabbits
- Development of Macroporous Chitosan Scaffolds for Eyelid Tarsus Tissue Engineering