J Periodontal Implant Sci.
2012 Feb;42(1):20-24. 10.5051/jpis.2012.42.1.20.
The effect of peri-implant bone exposure on soft tissue healing and bone loss in two adjacent implants
- Affiliations
-
- 1Department of Periodontology, The Institute of Oral Health Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. pkoyang@skku.edu
- 2Department of Oral and Maxillofacial Surgery, The Institute of Oral Health Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2212081
- DOI: http://doi.org/10.5051/jpis.2012.42.1.20
Abstract
- PURPOSE
The purpose of this study was to evaluate the soft tissue and bone change around two adjacent implants in one-stage implant surgery.
METHODS
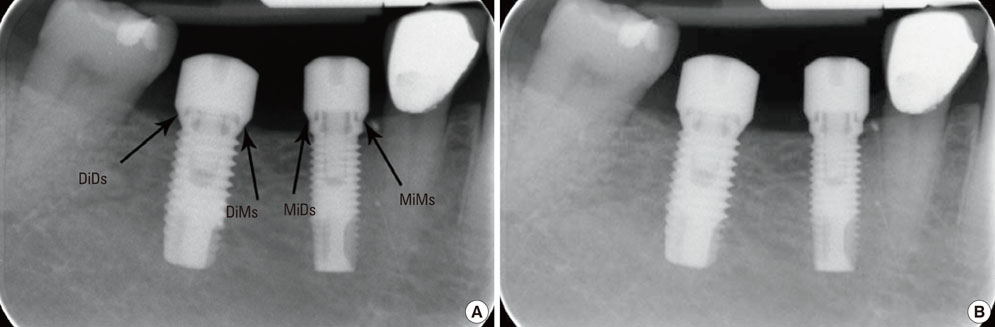
Eleven subjects (7 males, 4 females) who were needed placement of 2 adjacent implants in the molar area were included. The two implants were placed with the platform at the level of the alveolar crest. The interproximal bone between the 2 implants was not covered with gingiva. After surgery, an alginate impression was taken to record the gingival shape and radiographs were taken to evaluate implant placement. Using a master cast, the gingival height was measured at baseline, 4 weeks, and 12 weeks. In the radiograph, the alveolar bone level was measured at the mesial and distal side of both implants at baseline and 12 weeks.
RESULTS
The exposed bone was covered with gingiva at both 4 and 12 weeks. Loss of alveolar bone around implants was found in all areas. The alveolar bone level in the exposed bone area did not differ from that in the non-exposed area.
CONCLUSIONS
This study showed that the alveolar bone level and gingival height around 2 adjacent implants in the exposed bone area did not differ from that in unexposed bone area.
Keyword
MeSH Terms
Figure
Reference
-
1. Lindhe J, Lang NP, Karring T. Clinical periodontology and implant dentistry. 2008. 5th ed. Oxford: Blackwell Munksgaard.2. Becker W, Ochsenbein C, Tibbetts L, Becker BE. Alveolar bone anatomic profiles as measured from dry skulls. Clinical ramifications. J Clin Periodontol. 1997. 24:727–731.3. Choquet V, Hermans M, Adriaenssens P, Daelemans P, Tarnow DP, Malevez C. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001. 72:1364–1371.
Article4. Kois JC, Kan JY. Predictable peri-implant gingival aesthetics: surgical and prosthodontic rationales. Pract Proced Aesthet Dent. 2001. 13:691–698.
Article5. Salama H, Salama M, Garber D, Adar P. Developing optimal peri-implant papillae within the esthetic zone: guided soft tissue augmentation. J Esthet Dent. 1995. 7:125–129.
Article6. Tarnow D, Elian N, Fletcher P, Froum S, Magner A, Cho SC, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003. 74:1785–1788.
Article7. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992. 63:995–996.
Article8. Esposito M, Ekestubbe A, Gröndahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Brånemark implants. Clin Oral Implants Res. 1993. 4:151–157.
Article9. Palacci P, Ericsson I, Engstrand P, Rangert B. Optimal implant positioning & soft tissue management for the Branemark system. 1996. Chicago: Quintessence Publisher.10. Park KB. Current soft tissue management in implant dentistry. 1999. Seoul: Narae Publishing.11. Lee EK, Herr Y, Kwon YH, Shin SI, Lee DY, Chung JH. I-shaped incisions for papilla reconstruction in second stage implant surgery. J Periodontal Implant Sci. 2010. 40:139–143.
Article12. Yang SM, Shin SY, Kye SB. Relationship between implant stability measured by resonance frequency analysis (RFA) and bone loss during early healing period. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008. 105:e12–e19.
Article13. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981. 10:387–416.
Article14. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986. 1:11–25.
Article15. Hermann F, Lerner H, Palti A. Factors influencing the preservation of the periimplant marginal bone. Implant Dent. 2007. 16:165–175.16. Oh TJ, Yoon J, Misch CE, Wang HL. The causes of early implant bone loss: myth or science? J Periodontol. 2002. 73:322–333.17. Berglundh T, Lindhe J. Dimension of the periimplant mucosa. Biological width revisited. J Clin Periodontol. 1996. 23:971–973.
Article18. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000. 71:546–549.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Advanced peri-implantitis cases with radical surgical treatment
- The effects of tissue punch diameter on healing around implants in flapless implant surgery
- Effect of the early exposure of cover screws on the survival rate of implants
- Influence of soft tissue and bone thickness on the dimensional change of peri-implant soft tissues: A clinical follow-up study
- Treatment of Peri-implantitis: Cases Report