J Korean Soc Spine Surg.
2013 Mar;20(1):1-7. 10.4184/jkss.2013.20.1.1.
Correlation of Adjacent Segmental Disease with Tilt Angles of the Upper and Lower Instrumented Vertebra in the Degenerative Lumbar Scoliosis
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungnam National University, School of Medicine, Daejeon, Korea. jyyang@cnu.ac.kr
- KMID: 2209494
- DOI: http://doi.org/10.4184/jkss.2013.20.1.1
Abstract
- STUDY DESIGN: Retrospective study.
OBJECTIVES
To evaluate the correlation of adjacent segmental disease with tilt angles of the upper and lower instrumented vertebra after instrumented posterolateral fusion for degenerative lumbar scoliosis. SUMMARY OF LITERATURE REVIEW: There has been no study of radiologic measurement and decision of fusion level using the angle of pedicle screws inserted for treatment of degenerative lumbar scoliosis.
MATERIALS AND METHODS
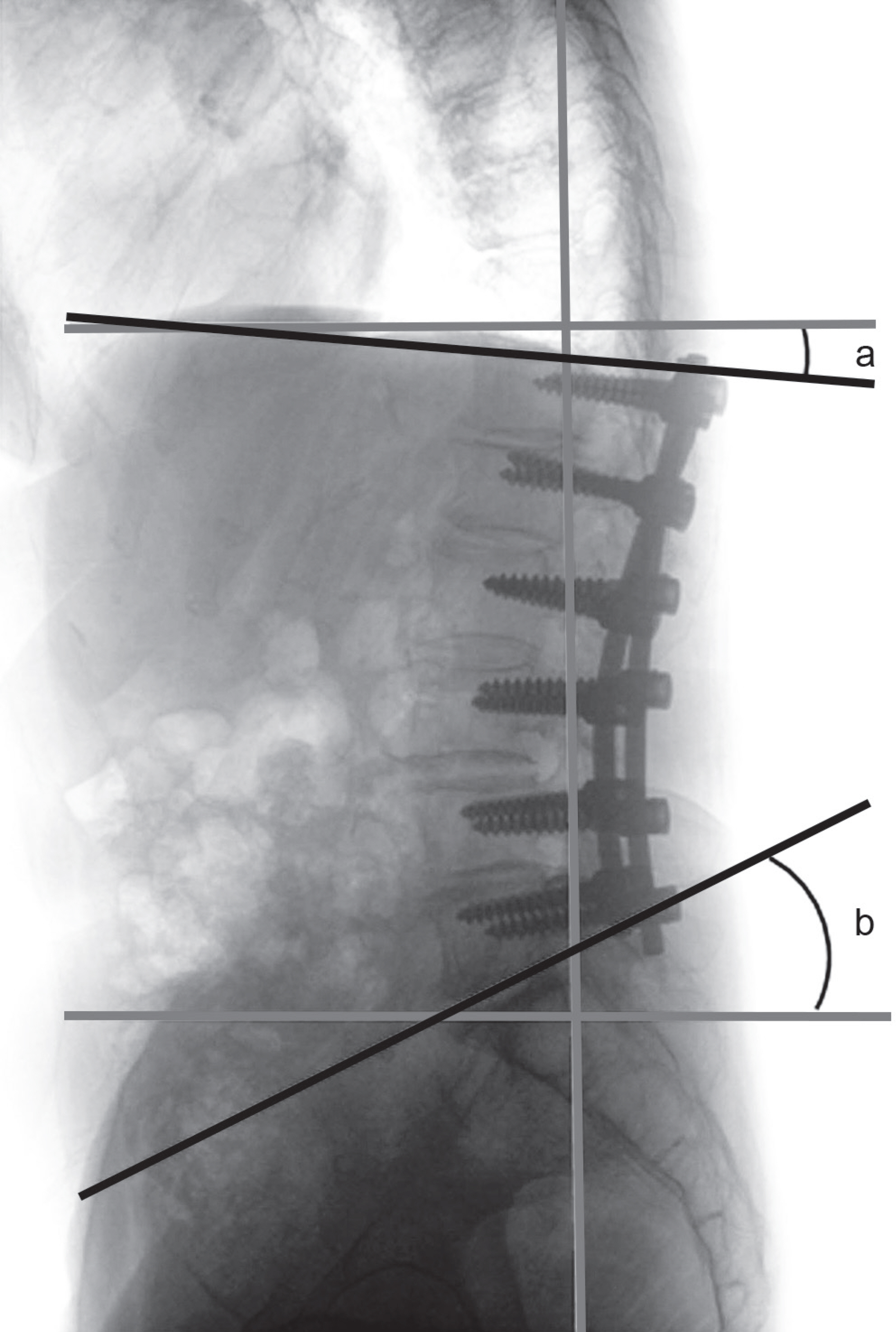
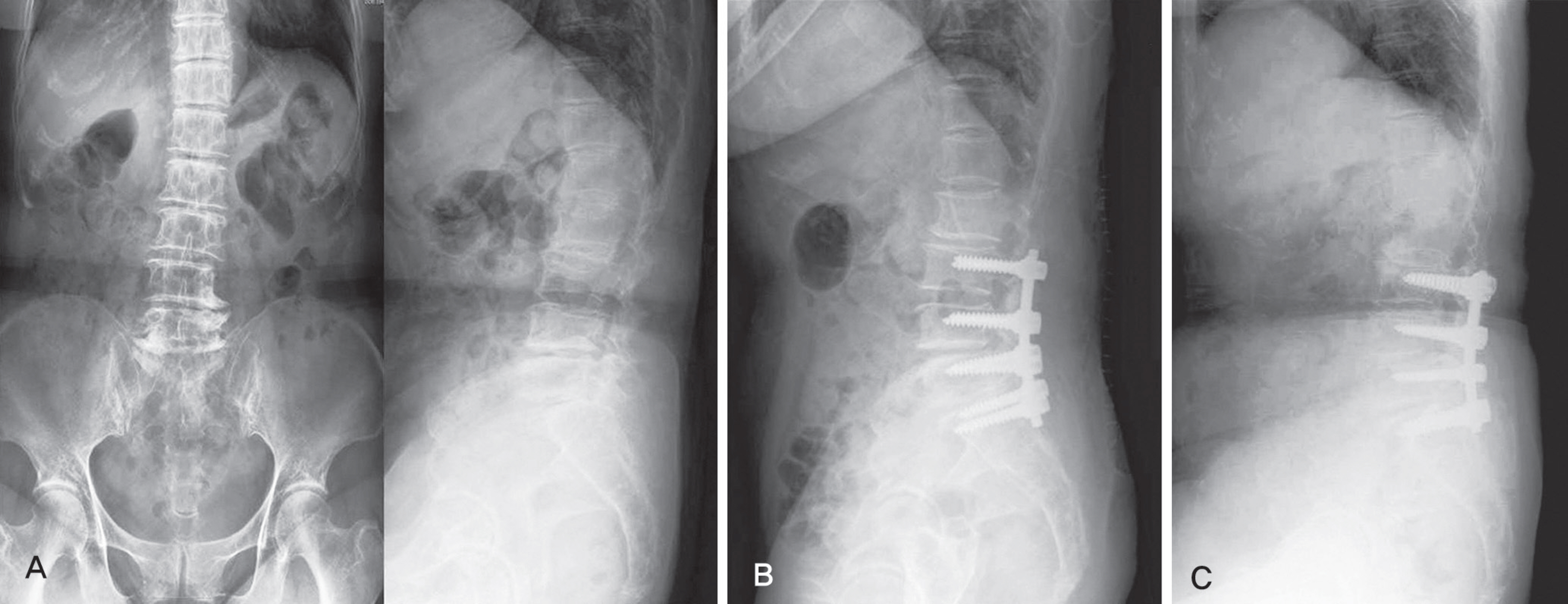
From 2004 to 2008, 74 patients that underwent decompression and posterolateral fusion for degenerative lumbar scoliosis were included in this study. In all cases, instrumentation and posterolateral fusion were both performed. The sex ratio was 31:43, the mean age was 68.7 years and the mean follow up duration was 37.4 months. The angle between each upper end plate of the upper vertebral body and lower end plate of the lower vertebral body of the fusion, and the line parallel to the axis of the sagittal line of vertebrae was each defined as UIV-a and LIV-b. The correlation of development of adjacent segment disease and UIV-a, and LIV-b angle was investigated.
RESULTS
Sum of the absolute value of UIV-a and LIV-b had a statistically significant positive correlation with that of adjacent segment disease. Also, UIV-a alone, had a statistically positive correlation with the development of proximal adjacent segment disease.
CONCLUSIONS
Since it is proven that adjacent segment disease has positive correlation with the sum of the absolute value of UIV-a and LIV-b, the extent of fusion should be adjusted to make the line parallel to the line perpendicular to the sagittal surface.
Keyword
MeSH Terms
Figure
Reference
-
1.Epstein JA., Epstein BS., Jones MD. Symptomatic lumbar scoliosis with degenerative changes in the elderly. Spine (Phila Pa 1976). 1979. 4:542–7.
Article2.Song KJ., Choi BW., Song JH., Kim GH. The Causes of Re-vision Arthrodesis for the Degenerative Changes at the Adjacent Segment after Lumbosacral Fusion for Degenerative Lumbar Diseases. J Korean Soc Spine Surg. 2008. 15:230–5.
Article3.Grubb SA., Lipscomb HJ. Diagnostic findings in painful adult scoliosis. Spine (Phila Pa 1976). 1992. 17:518–27.
Article4.Benner B., Ehni G. Degenerative lumbar scoliosis. Spine (Phila Pa 1976). 1979. 4:548–52.
Article5.Kostuik JP. Decision making in adult scoliosis. Spine (Phila Pa 1976). 1979. 4:521–5.
Article6.Aebi M. Correction of degenerative scoliosis of the lumbar spine. A preliminary report. Clin Orthop Relat Res. 1988. 232:80–6.7.Nash CL Jr., Moe JH. A study of vertebral rotation. J Bone Joint Surg Am. 1969. 51:223–9.
Article8.Hilibrand AS., Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequence of spinal fusion? Spine J. 2004. 4(6 Suppl):190S–4S.9.Booth KC., Bridwell KH., Eisenberg BA., Baldus CR., Lenke LG. Minimum 5-year results of degenerative spondylolis-thesis treated with decompression and instrumented posterior fusion. Spine (Phila Pa 1976). 1999. 24:1721–7.
Article10.Lenke LG., Bridwell KH., Bullis D., Betz RR., Baldus C., Schoenecker PL. Results of in situ fusion for isthmic spon-dylolisthesis. J Spinal Disord. 1992. 5:433–42.
Article11.Kumar MN., Jacquot F., Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine surgery for denerative disc disease. Eur Spine J. 2001. 10:309–13.12.Ahn DK., Lee S., Jeong KW., Park JS., Cha SK., Park HS. Adjacent Segment failure after Lumbar Spine Fusion: Con-trolled Study for Risk Factors. J Korean Orthop Assoc. 2005. 40:203–8.
Article13.Wu CH., Wong CB., Chen LH., Niu CC., Tsai TT., Chen WJ. Instrumented posterior lumbar interbody fusion for patients with degenerative lumbar scoliosis. J Spinal Disord Tech. 2008. 21:310–5.
Article14.Rohlman A., Neller S., Bergmann G., Graichen F., Claes L., Wilke HJ. Effect of an internal fixator and a bone graft on instersegmental spinal motion and intradiscal pressure in the adjacent region. Eur Spine J. 2001. 10:301–8.15.Gillet P. The fate of the adjacent motion segment after lum-bar fusion. J Spinal Disord Tech. 2003. 16:338–45.16.Lee CK. Lumbar spinal instability (olisthesis) after exten-sive posterior spinal decompression. Spine (Phila Pa 1976). 1983. 8:429–33.
Article17.Schlegel JD., Smith JA., Schleusener RL. Lumbar motion segment patholoty adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine (Phila Pa 1976). 1996. 21:970–81.18.Simmons ED., Simmons EH. Spinal stenosis with scoliosis. Spine (Phila Pa 1976). 1992. 17(6 Suppl):S117–20.
Article19.Herkowitz HN., Kurz LT. Degenerative lumbar spondylo-listhesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrosis. J Bone Joint Surg Am. 1991. 73:802–8.20.Cho KJ., Park SL., Kim MG., Yoon YH., Lee JS., Suk SI. Proximal Adjacent Segment Disease following Posterior Instrumentation and Fusion for Degenerative Lumbar Scoliosis. J Korean Orthop Assoc. 2009. 44:109–17.
Article21.Shufflebarger H., Suk SI., Mardjetko S. Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine (Phila Pa 1976). 2006. 31(19 Suppl):S185–94.22.Tsuchiya K., Bridwell KH., Kuklo TR., Lenke LG., Baldus C. Minimum 5-year analysis L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006. 31:303–8.23.Edwards CC 2nd., Bridwell KH., Patel A, et al. Thoraco-lumbar deformity arthrodesis to L5 in adults: the fate of the L5-S1 disc. Spine (Phila Pa 1976). 2003. 28:2122–31.
Article24.Dekutoski MB., Schendel MJ., Ogilvie JW., Olsewski JM., Wallace LJ., Lewis JL. Compression of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine (Phila Pa 1976). 1994. 19:1745–51.25.Grouw AV., Nadel CI., Weieman RJ., Lowell HA. Long term follow-up of patients with idiopathic scoliosis treated surgi-cally: a preliminary subjective study. Clin Orthop Relat Res. 2001. 117:197–201.
Article26.Cho JL., Choi SW., Lee JM., Park YS. The Changes of Ad-jacent Segments after Long Segment Posterolateral Fusion: Comparative Study of 3 year versus over the 7 year Follow-up Patients. J Korean Orthop Assoc. 2005. 40:38–43.
Article27.Lee CK., Langrana NA. Lumbosacral spinal fusion. A bio-mechanical study. Spine (Phila Pa 1976). 1984. 9:574–81.
Article28.Weinhoffer SL., Guyer RD., Herbert M., Griffith SL. Intra-discal pressure measurements above an instrumented fusion. A cadaveric study. Spine (Phila Pa 1976). 1995. 20:526–31.29.Cunningham BW., Kotani Y., McNulty PS., Cappuccino A., McAfee PC. The effect of spinal destabilization and instrumentation on lumbar intradiscal pressure: an in vitro bio-mechanical analysis. Spine (Phila Pa 1976). 1997. 22:2655–63.30.Yang SH., Chen PQ. Proximal kyphosis after short posterior fusion for thoracolumbar scoliosis. Clin Orthop Relat Res. 2003. 411:152–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proximal Adjacent Segment Disease following Posterior Instrumentation and Fusion for Degenerative Lumbar Scoliosis
- Correction of Curve and Determination of Fixation Segment in Degenerative Lumbar Scoliosis
- Progression of Preoperative Degeneration of the Adjacent Segmentafter Instrumented Lumbar Arthrodesis
- Preliminary Report on Usefulness of Adjacent Interspinous Stabilization using Interspinous Spacer Combined with Posterior Lumbosacral Spinal Fusion in Degenerative Lumbar Disease
- Changes in Vertebral Axial Rotation after Thoracoscopic Scoliosis Correction