J Korean Soc Transplant.
2015 Dec;29(4):238-241. 10.4285/jkstn.2015.29.4.238.
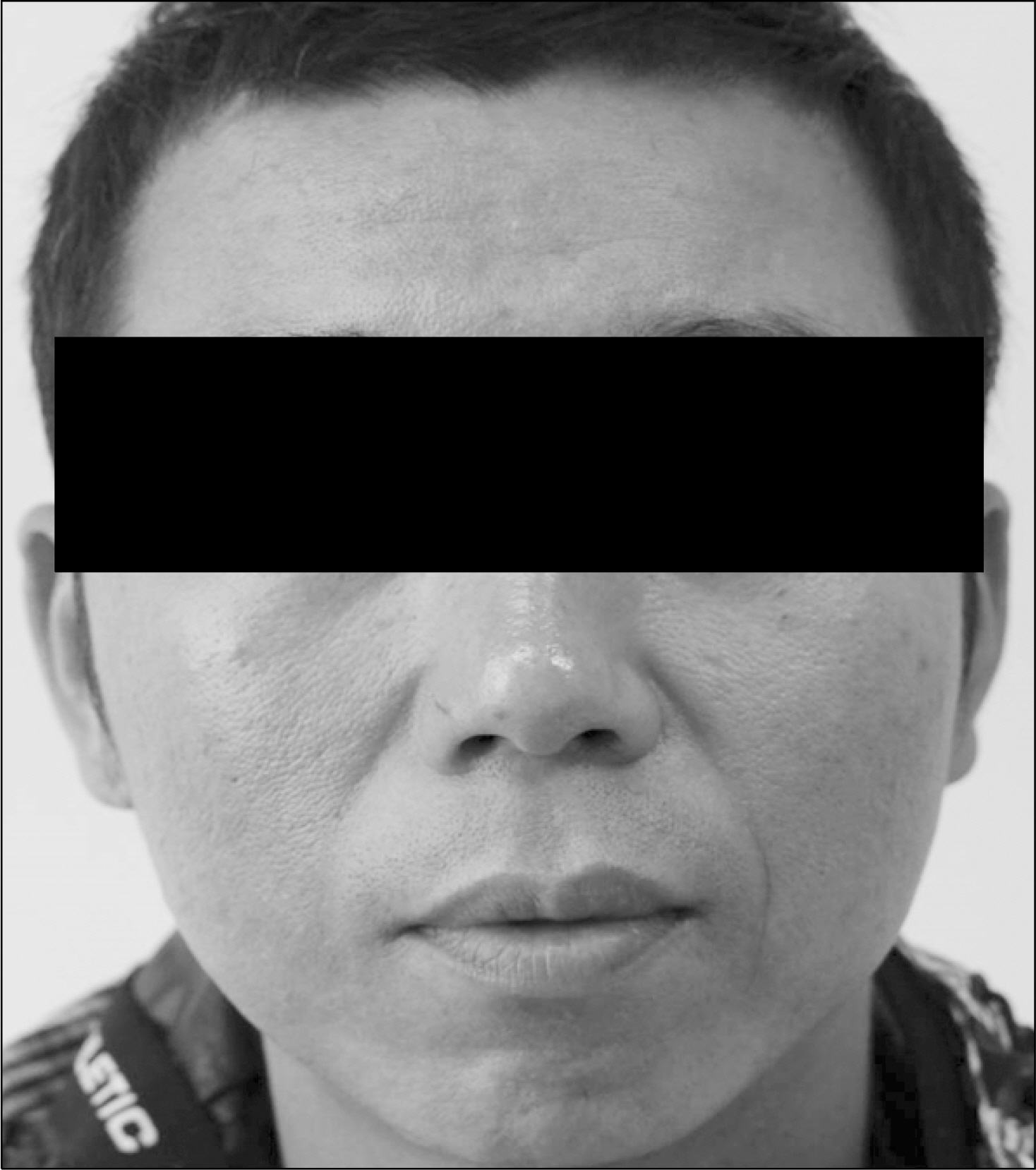
Kidney Transplant Patient with a Facial Redness
- Affiliations
-
- 1Department of Internal Medicine, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea. parksk@jbnu.ac.kr
- 2Department of Surgery, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea.
- KMID: 2202610
- DOI: http://doi.org/10.4285/jkstn.2015.29.4.238
Abstract
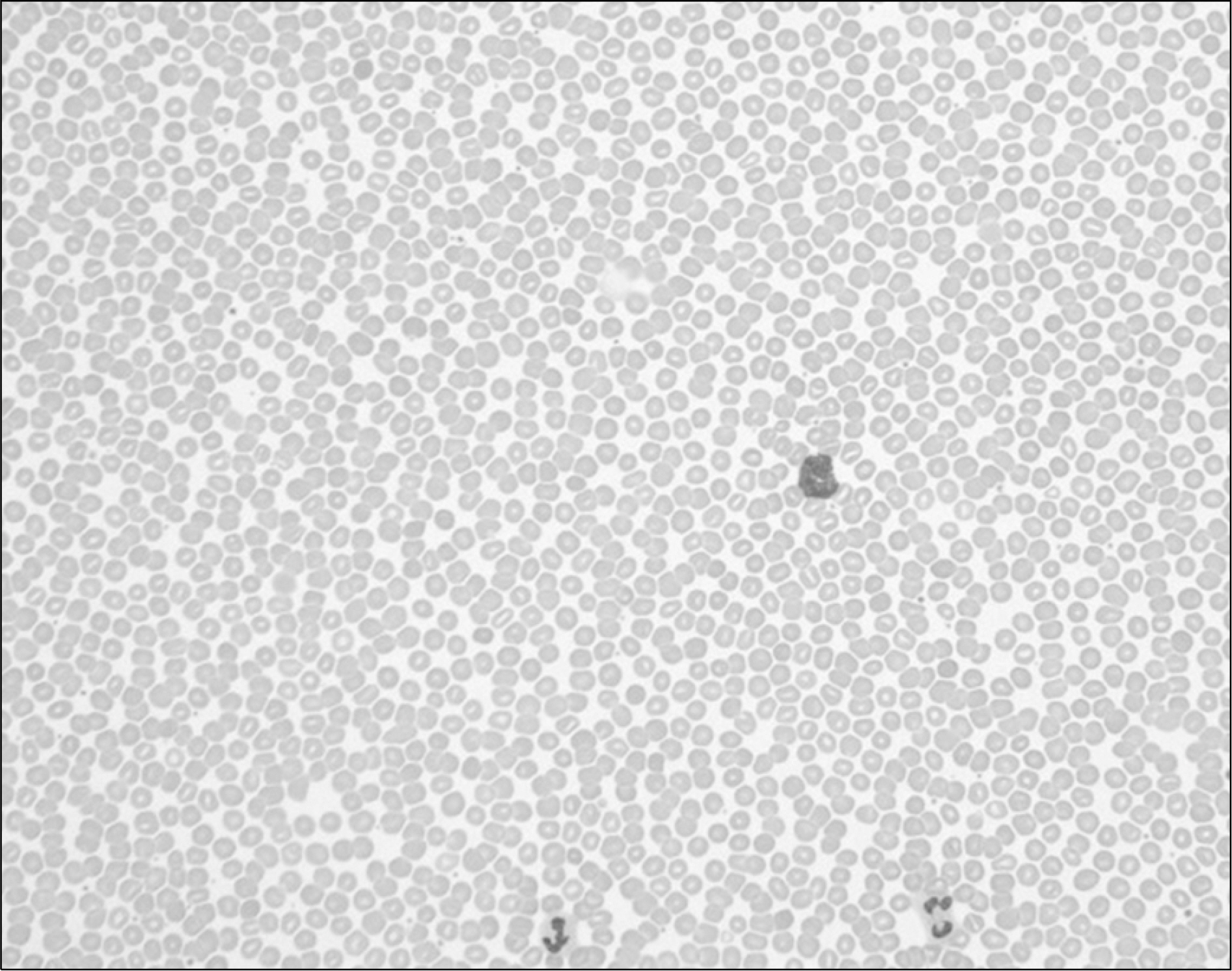
- Posttransplant erythrocytosis (PTE) is a common complication of renal transplantation, which can occur in approximately 10% to 15% of renal transplant patients and usually affects males with relatively good renal function. It is also associated with an increased incidence of thromboembolic events. Clinical manifestations of PTE include malaise, headache, plethora, lethargy, and dizziness. It is correlated with use of cyclosporin, gender, posttransplant renal function, and type of antihypertensive medication. The angiotensin receptor blocker (ARB) or angiotensin-converting enzyme inhibitor is preferred as an initial treatment for PTE because these agents are effective and reasonably safe in the majority of patients with PTE, and can also provide a necessary antihypertensive effect for kidney transplant patients. We report here on a 35-year-old male who had erythrocytosis after renal transplantation. After renal transplantation, his level of hemoglobin was 21 g/dL. We treated this patient with ARB and his symptoms and signs have been completely relieved.
MeSH Terms
Figure
Reference
-
References
1). Gaston RS, Julian BA, Curtis JJ. Posttransplant erythrocytosis: an enigma revisited. Am J Kidney Dis. 1994; 24:1–11.
Article2). Vlahakos DV, Marathias KP, Agroyannis B, Madias NE. Posttransplant erythrocytosis. Kidney Int. 2003; 63:1187–94.
Article3). Choi GS, Kim DJ, Han YS, Kwon CH, Kim SJ, Joh JW. Severe erythrocytosis after renal transplantation: report of one case. J Korean Soc Transplant. 2006; 20:121–3. (최규성, 김두진, 한영석, 권준혁, 김성주, 조재원. 신장 이식술 후 발생한 심한 적혈구 증가증 1예. 대한이식학회지 2006;20: 121–3.).4). Kessler M, Hestin D, Mayeux D, Mertes PM, Renoult E. Factors predisposing to postrenal transplant erythrocytosis. A prospective matched-pair control study. Clin Nephrol. 1996; 45:83–9.5). Aeberhard JM, Schneider PA, Vallotton MB, Kurtz A, Leski M. Multiple site estimates of erythropoietin and renin in polycythemic kidney transplant patients. Transplantation. 1990; 50:613–6.
Article6). Esposito R, Giammarino A, De Blasio A, Martinelli V, Cirillo F, Scopacasa F, et al. Ramipril in postrenal transplant erythrocytosis. J Nephrol. 2007; 20:57–62.7). Wickre CG, Norman DJ, Bennison A, Barry JM, Bennett WM. Postrenal transplant erythrocytosis: a review of 53 patients. Kidney Int. 1983; 23:731–7.
Article8). Rell K, Koziak K, Jarzyo I, Lao M, Gaciong Z. Correction of posttransplant erythrocytosis with enalapril. Transplantation. 1994; 57:1059–63.
Article9). Macdougall IC, Karim S, Amos R, Baker LR, Raine AE. Polycythemia in renal transplant recipients is not mediated solely by enhanced erythropoietin activity. J Am Soc Nephrol. 1992; 3:428.10). Tatman AJ, Tucker B, Amess JA, Cattell WR, Baker LR. Erythraemia in renal transplant recipients treated with cyclosporin. Lancet. 1988; 1:1279.
Article11). Ifudu O, Uribarri J, Rajwani I, Vlacich V, Reydel K, Delos-reyes G, et al. Gender modulates responsiveness to recombinant erythropoietin. Am J Kidney Dis. 2001; 38:518–22.
Article12). Einollahi B, Lessan-Pezeshki M, Nafar M, Pour-Reza-Gholi F, Firouzan A, Farhangi F, et al. Erythrocytosis after renal transplantation: review of 101 cases. Transplant Proc. 2005; 37:3101–2.
Article13). Spieker C, Barenbrock M, Tepel M, Zidek W. Long-term effect on hypertension of phlebotomy in posttransplant erythrocytosis. Transplant Proc. 1992; 24:2742–4.14). Garvin PJ, Reese JC, Lindsey L, Aridge DL, Domoto DT, Ballal S. Bilateral nephrectomy for posttransplant erythrocytosis: indications and result. Clin Transplant. 1991; 5:313–7.15). Glicklich D, Burris L, Urban A, Tellis V, Greenstein S, Schechner R, et al. Angiotensin-converting enzyme inhibition induces apoptosis in erythroid precursors and affects insulinlike growth factor-1 in posttransplantation erythrocytosis. J Am Soc Nephrol. 2001; 12:1958–64.
Article16). Jeon GH, Park SK, Kim SW, Rhee SR. Effect of enalapril treatment on erythrocytosis after renal transplantation. J Korean Surg Soc. 1997; 52:572–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Local Clinic Experience of Facial Redness in Koreans
- Kidney transplant in a pediatric patient with double inferior vena cava: a case report
- Approach to kidney transplant patients with pre-transplant malignancy
- A Concept Analysis of Compliance in Kidney Transplant Recipient Including Compliance with Immunosuppressive Medication
- Rhabdomyolysis Induced by Hypothyroidism in a Kidney Transplant Recipient