J Lipid Atheroscler.
2014 Jun;3(1):29-37. 10.12997/jla.2014.3.1.29.
Abdominal and Pericardial Fat in Patients with and without Coronary Artery Disease: Computed Tomography Study
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 2Division of Cardiology, Department of Medicine, Chungbuk National University Hospital, Cheongju, Korea. kdwoon@chungbuk.ac.kr
- 3Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Division of Cardiology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jepark@gmail.com
- KMID: 2198358
- DOI: http://doi.org/10.12997/jla.2014.3.1.29
Abstract
OBJECTIVE
There has been a limited investigation looking into the correlation between pericardial fat and abdominal fat with coronary artery disease (CAD) as measured by coronary computed tomographic angiography (CCTA). We proposed that the volume of pericardial fat is larger in patients with CAD than in patients without CAD, and sought to determine which abdominal adiposity index best correlated with pericardial fat volume.
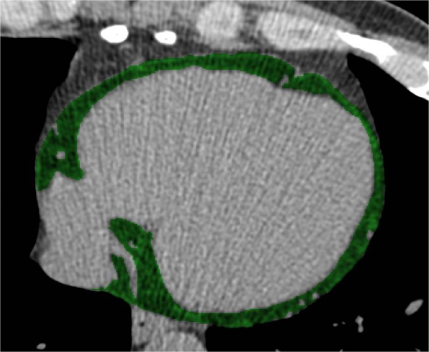
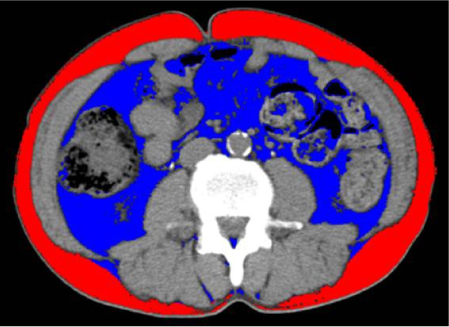
METHODS
Participants were examined using CCTA between October 2007 and January 2008. All participants had no previous history of CAD. Pericardial adipose tissue (PAT) volume, abdominal total adipose tissue volume, abdominal subcutaneous adipose tissue volume, and abdominal visceral adipose tissue (AVAT) volume were measured using CCTA.
RESULTS
Fifty patients (26.5%) demonstrated CAD, and 139 patients did not demonstrate CAD by CCTA. PAT volume in patients with CAD was larger than that of patients without CAD (173.2+/-64.2 cm3 vs. 147.6+/-50.4 cm3, p<0.01). However, indices of abdominal adiposity were not significantly different between the two groups. Using multivariable analysis, independent predictors of CAD were PAT volume (odds ratio [OR] 1.01, 95% confidence interval [CI] 1.00-1.02, p=0.04), coronary artery calcium score (OR 1.01, 95% CI 1.00-1.01, p<0.01), and typical chest pain (OR 4.88, 95% CI 1.47-16.21, p=0.01). AVAT volume showed a linear correlation with PAT volume.
CONCLUSION
PAT volume was an independent predictor of CAD as measured by CCTA. PAT volume was also well correlated with the AVAT volume among the indices of abdominal adiposity.
Keyword
MeSH Terms
Figure
Reference
-
1. Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983; 67:968–977.
Article2. Seo J, Kim DS, Kwon HM, Jang Y, Kim HS, Cho H, et al. Severity of coronary artery disease and visceral fat obesity. Korean Circ J. 1998; 28:1176–1184.
Article3. Sowers JR. Obesity as a cardiovascular risk factor. Am J Med. 2003; 115:Suppl 8A. 37S–41S.
Article4. Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007; 116:39–48.
Article5. Ahn SG, Lim HS, Joe DY, Kang SJ, Choi BJ, Choi SY, et al. Relationship of epicardial adipose tissue by echocardiography to coronary artery disease. Heart. 2008; 94:e7.
Article6. Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008; 117:605–613.
Article7. Schroeder S, Achenbach S, Bengel F, Burgstahler C, Cademartiri F, de Feyter P, et al. Cardiac computed tomography: indications, applications, limitations, and training requirements: report of a Writing Group deployed by the Working Group Nuclear Cardiology and Cardiac CT of the European Society of Cardiology and the European Council of Nuclear Cardiology. Eur Heart J. 2008; 29:531–556.
Article8. Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008; 358:1336–1345.
Article9. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990; 15:827–832.
Article10. Ohashi N, Yamamoto H, Horiguchi J, Kitagawa T, Kunita E, Utsunomiya H, et al. Association between visceral adipose tissue area and coronary plaque morphology assessed by CT angiography. JACC Cardiovasc Imaging. 2010; 3:908–917.
Article11. Hoffmann U, Truong QA, Schoenfeld DA, Chou ET, Woodard PK, Nagurney JT, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012; 367:299–308.
Article12. Cheng VY, Dey D, Tamarappoo B, Nakazato R, Gransar H, Miranda-Peats R, et al. Pericardial fat burden on ECG-gated noncontrast CT in asymptomatic patients who subsequently experience adverse cardiovascular events. JACC Cardiovasc Imaging. 2010; 3:352–360.
Article13. Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003; 108:2460–2466.
Article14. Kim TH, Yu SH, Choi SH, Yoon JW, Kang SM, Chun EJ, et al. Pericardial fat amount is an independent risk factor of coronary artery stenosis assessed by multidetector-row computed tomography: the Korean Atherosclerosis Study 2. Obesity (Silver Spring). 2011; 19:1028–1034.
Article15. Bachar GN, Dicker D, Kornowski R, Atar E. Epicardial adipose tissue as a predictor of coronary artery disease in asymptomatic subjects. Am J Cardiol. 2012; 110:534–538.
Article16. Thanassoulis G, Massaro JM, Hoffmann U, Mahabadi AA, Vasan RS, O'Donnell CJ, et al. Prevalence, distribution, and risk factor correlates of high pericardial and intrathoracic fat depots in the Framingham heart study. Circ Cardiovasc Imaging. 2010; 3:559–566.
Article17. Sacks HS, Fain JN. Human epicardial fat: what is new and what is missing? Clin Exp Pharmacol Physiol. 2011; 38:879–887.
Article18. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002; 105:1135–1143.
Article19. Tamarappoo B, Dey D, Shmilovich H, Nakazato R, Gransar H, Cheng VY, et al. Increased pericardial fat volume measured from noncontrast CT predicts myocardial ischemia by SPECT. JACC Cardiovasc Imaging. 2010; 3:1104–1112.
Article20. Greif M, Becker A, von Ziegler F, Lebherz C, Lehrke M, Broedl UC, et al. Pericardial adipose tissue determined by dual source CT is a risk factor for coronary atherosclerosis. Arterioscler Thromb Vasc Biol. 2009; 29:781–786.
Article21. Wheeler GL, Shi R, Beck SR, Langefeld CD, Lenchik L, Wagenknecht LE, et al. Pericardial and visceral adipose tissues measured volumetrically with computed tomography are highly associated in type 2 diabetic families. Invest Radiol. 2005; 40:97–101.
Article22. Konishi M, Sugiyama S, Sugamura K, Nozaki T, Ohba K, Matsubara J, et al. Association of pericardial fat accumulation rather than abdominal obesity with coronary atherosclerotic plaque formation in patients with suspected coronary artery disease. Atherosclerosis. 2010; 209:573–578.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Coronary Artery Bypass Graft Patency Using Multidetector Computed Tomography
- Partial Pericardial Defect Incidentally Discovered During Coronary Bypass Surgery
- A Case of Partial Congenital Pericardial Defect Presenting as Acute Coronary Syndrome
- Unusual Coronary Artery Fistula: Left Anterior Descending Coronary Artery - Left Ventricular Fistula Diagnosed by ECG-Gated Multi-Detector Row Coronary CT Angiography
- Pericardial Recess: Computed Tomography Findings of Varying Disorders