J Korean Med Assoc.
2011 May;54(5):523-529. 10.5124/jkma.2011.54.5.523.
Reemerging skin disease caused by arthropods II: louse
- Affiliations
-
- 1Department of Environmental and Tropical Medicine, Konkuk University School of Medicine, Chungju, Korea.
- 2Department of Pediatrics, Ajou University School of Medicine, Suwon, Korea. kisoopai@ajou.ac.kr
- KMID: 2190714
- DOI: http://doi.org/10.5124/jkma.2011.54.5.523
Abstract
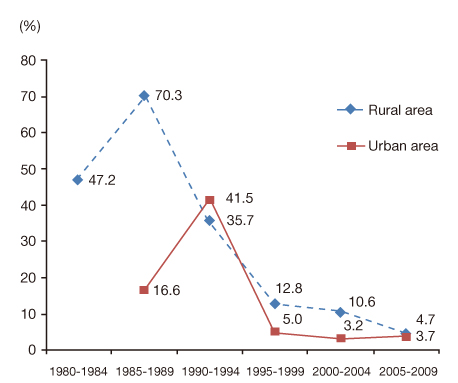
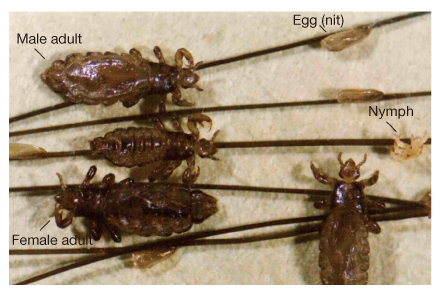
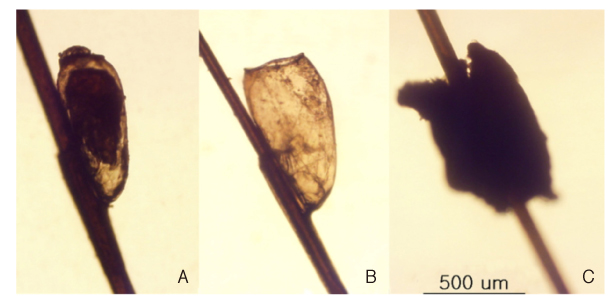
- The aim of this article is to provide guidelines to diagnosis and therapeutics for HLI in Korea. Head lice infestation (HLI) caused by Pediculus humanus capitis is still common in Korean children in spite of an improvement since the 1980s in the country's economic status and the concepts of hygiene. HLI is troublesome and, if not treated, can lead to secondary bacterial infection as a result of scratching of the irritated scalp induced by an inflammatory reaction to injected saliva or anticoagulant. In addition, HLI causes social and psychological problems as well as physical symptoms. Confirmation of the HLI depends on identification of adult lice, nymphs, or viable nits. Nits are more commonly found at the nape of the neck and retroauricular areas. The differential diagnosis includes hair casts, dandruff, and debris by hair spray. Few chemical shampoos such as those containing lindane or pyrethrin are currently available in Korea. Although HLI is an important public health issue in Korea, little information is available on HLI. Medical doctors, school nurses, and teachers should be acquainted with HLI for the successful control of this disease, which is distressing a number of children covertly.
MeSH Terms
Figure
Cited by 1 articles
-
Chemotherapeutic drugs for common parasitic diseases in Korea
Sun Huh
J Korean Med Assoc. 2013;56(6):513-522. doi: 10.5124/jkma.2013.56.6.513.
Reference
-
1. Araujo A, Ferreira LF, Guidon N, Maues Da Serra Freire N, Reinhard KJ, Dittmar K. Ten thousand years of head lice infection. Parasitol Today. 2000. 16:269.
Article2. Burkhart CN, Burkhart CG. Head lice: scientific assessment of the nit sheath with clinical ramifications and therapeutic options. J Am Acad Dermatol. 2005. 53:129–133.
Article3. Sim S, Lee IY, Lee KJ, Seo JH, Im KI, Shin MH, Yong TS. A survey on head lice infestation in Korea (2001) and the therapeutic efficacy of oral trimethoprim/sulfamethoxazole adding to lindane shampoo. Korean J Parasitol. 2003. 41:57–61.
Article4. Oh JM, Lee IY, Lee WJ, Seo M, Park SA, Lee SH, Seo JH, Yong TS, Park SJ, Shin MH, Pai KS, Yu JR, Sim S. Prevalence of pediculosis capitis among Korean children. Parasitol Res. 2010. 107:1415–1419.
Article5. Lee SH, Oh CW, Chai JY. Head louse infestation among primary school children In Seosangun, Chungnam province. Korean J Parasitol. 1984. 22:141–143.
Article6. Kim TK, Park CP, Ho S. Head louse infestation among the students in Yongyang-gun, Kyongsangbuk-to. Korean J Parasitol. 1984. 22:273–276.
Article7. Pai KS, Park MS, Lee YS, Kim DH, Chung KS, Lee KY, Kim PK, Kim KY, Yong TS, Ree HI. The prevalence of head louse infestation among urban and rural children in Korea. Korean J Parasitol. 1989. 27:271–275.
Article8. Ree HI, Yong TS, Shin HJ, Shin CO, Lee IY, Seo SA, Seo JH, Chang JK, Lee DH, Im KI. Mass treatment of head louse infestation with Sumithrin powder in primary schools in Korea. Korean J Parasitol. 1992. 30:349–354.
Article9. Huh S, Pai KS, Lee SJ, Kim KJ, Kim NH. Prevalence of head louse infestation in primary school children in Kangwon-do, Korea. Korean J Parasitol. 1993. 31:67–69.
Article10. Hong HK, Kim CM, Lee JS, Lee WJ, Yang YC. Infestation rate of head lice in primary school children in Inchon, Korea. Korean J Parasitol. 1995. 33:243–244.
Article11. Ha YC, Heo JM, Kim HJ, Go GM, Lee SJ, Jeong SH, Ahn SI, Kim MC, Kim JE, Song HY, Park JW, Kim BS, Sohn WM. Infestation status of head louse and treatment with lindane shampoo in children of primary school and kindergarten in Chinju-shi, Kyongsangnam-do, Korea. Korean J Parasitol. 2000. 38:41–43.
Article12. de Berker D, Sinclair R. Getting ahead of head lice. Australas J Dermatol. 2000. 41:209–212.
Article13. Lebwohl M, Clark L, Levitt J. Therapy for head lice based on life cycle, resistance, and safety considerations. Pediatrics. 2007. 119:965–974.
Article14. Ko CJ, Elston DM. Pediculosis. J Am Acad Dermatol. 2004. 50:1–12.
Article15. Koch T, Brown M, Selim P, Isam C. Towards the eradication of head lice: literature review and research agenda. J Clin Nurs. 2001. 10:364–371.
Article16. Nash B. Treating head lice. BMJ. 2003. 326:1256–1257.
Article17. Jones KN, English JC 3rd. Review of common therapeutic options in the United States for the treatment of pediculosis capitis. Clin Infect Dis. 2003. 36:1355–1361.
Article18. Roberts RJ. Clinical practice. Head lice. N Engl J Med. 2002. 346:1645–1650.19. Heukelbach J, Wilcke T, Winter B, Feldmeier H. Epidemiology and morbidity of scabies and pediculosis capitis in resource-poor communities in Brazil. Br J Dermatol. 2005. 153:150–156.
Article20. Burkhart CN, Burkhart CG. Fomite transmission in head lice. J Am Acad Dermatol. 2007. 56:1044–1047.
Article21. Scott P, Middlefell LS, Fabbroni G, Mitchell DA. Interesting case: cervical lymphadenopathy, induced by head lice. Br J Oral Maxillofac Surg. 2005. 43:515.
Article22. Mumcuoglu KY, Klaus S, Kafka D, Teiler M, Miller J. Clinical observations related to head lice infestation. J Am Acad Dermatol. 1991. 25(2 Pt 1):248–251.
Article23. Speare R, Canyon DV, Melrose W. Quantification of blood intake of the head louse: Pediculus humanus capitis. Int J Dermatol. 2006. 45:543–546.
Article24. Guss DA, Koenig M, Castillo EM. Severe iron deficiency anemia and lice infestation. J Emerg Med. 2010. 07. 23. [Epub]. DOI: 10.1016/j.jemermed.2010.05.030.
Article25. Bonilla DL, Kabeya H, Henn J, Kramer VL, Kosoy MY. Bartonella quintana in body lice and head lice from homeless persons, San Francisco, California, USA. Emerg Infect Dis. 2009. 15:912–915.
Article26. Sasaki T, Poudel SK, Isawa H, Hayashi T, Seki N, Tomita T, Sawabe K, Kobayashi M. First molecular evidence of Bartonella quintana in Pediculus humanus capitis (Phthiraptera: Pediculidae), collected from Nepalese children. J Med Entomol. 2006. 43:110–112.
Article27. Leung AK, Fong JH, Pinto-Rojas A. Pediculosis capitis. J Pediatr Health Care. 2005. 19:369–373.
Article28. Frankowski BL. American Academy of Pediatrics guidelines for the prevention and treatment of head lice infestation. Am J Manag Care. 2004. 10:9 Suppl. S269–S272.29. Izri A, Chosidow O. Efficacy of machine laundering to eradi-cate head lice: recommendations to decontaminate washable clothes, linens, and fomites. Clin Infect Dis. 2006. 42:e9–e10.
Article30. Catala S, Junco L, Vaporaky R. Pediculus capitis infestation according to sex and social factors in Argentina. Rev Saude Publica. 2005. 39:438–443.
Article31. Meinking TL, Vicaria M, Eyerdam DH, Villar ME, Reyna S, Suarez G. Efficacy of a reduced application time of Ovide lotion (0.5% malathion) compared to Nix creme rinse (1% permethrin) for the treatment of head lice. Pediatr Dermatol. 2004. 21:670–674.
Article32. Hensel P. The challenge of choosing a pediculicide. Public Health Nurs. 2000. 17:300–304.
Article33. Akisu C, Delibas SB, Aksoy U. Albendazole: single or combination therapy with permethrin against pediculosis capitis. Pediatr Dermatol. 2006. 23:179–182.
Article34. Burns DA. Action of cotrimoxazole on head lice. Br J Dermatol. 1987. 117:399–400.
Article35. Roberts RJ, Casey D, Morgan DA, Petrovic M. Comparison of wet combing with malathion for treatment of head lice in the UK: a pragmatic randomised controlled trial. Lancet. 2000. 356:540–544.
Article36. Sim S, Lee WJ, Yu JR, Lee IY, Lee SH, Oh SY, Seo M, Chai JY. Risk factors associated with head lice infestation in Korea. Korean J Parasitol. 2011. 49:95–98.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reemerging skin disease caused by arthropods I: scabies
- Household Arthropod Allergens in Korea
- Head louse infestation among primary school children in Seosan-gun, Chungnam Province
- International Cooperation in the Control and Prevention of Emerging and Reemerging Infectious Diseases
- Head louse infestation among school children in Sanbuk-myon, Mungyong-gun, Kyongsangbuk-do (1985)