J Korean Orthop Assoc.
2012 Aug;47(4):293-298. 10.4055/jkoa.2012.47.4.293.
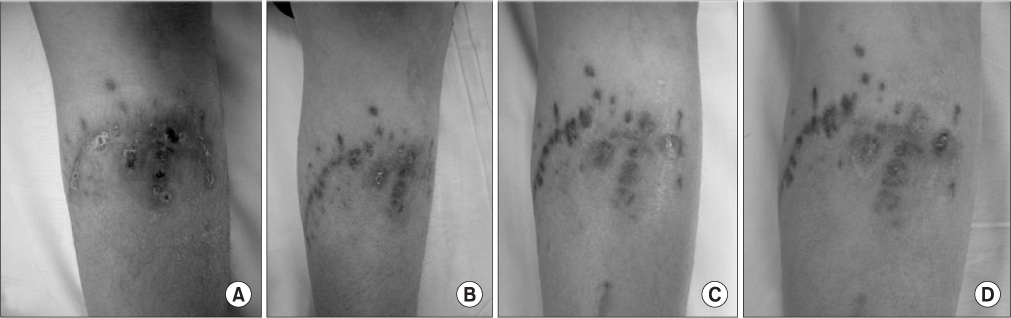
Chronic Granulomatous Infection of Soft Tissue Complicated by Trauma of a Lower Leg
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kwangju Christian Hospital, Gwangju, Korea. stemcellchoi@yahoo.co.kr
- KMID: 2185377
- DOI: http://doi.org/10.4055/jkoa.2012.47.4.293
Abstract
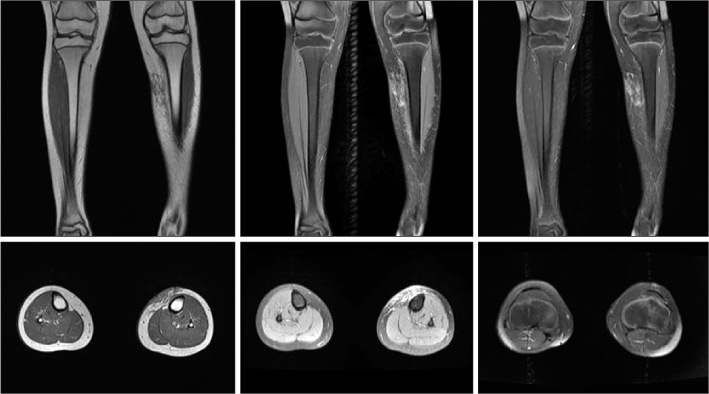
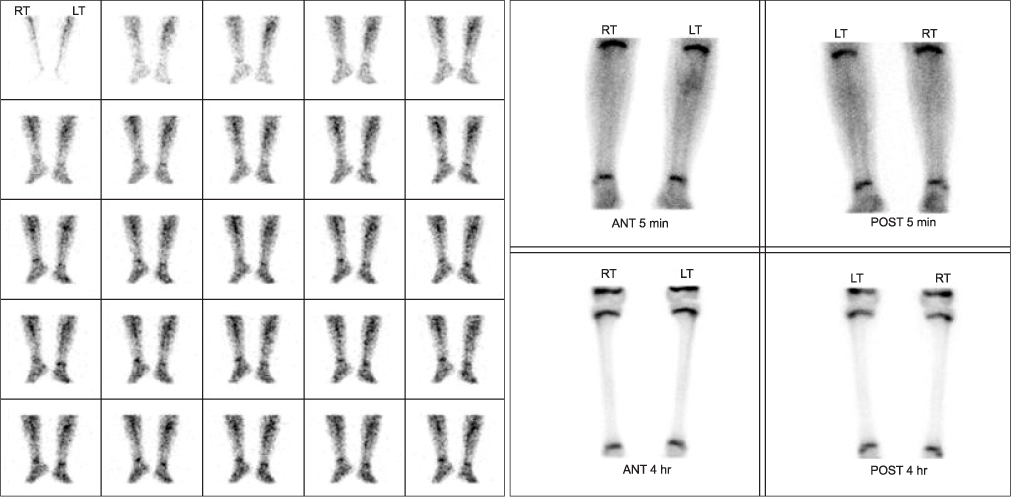
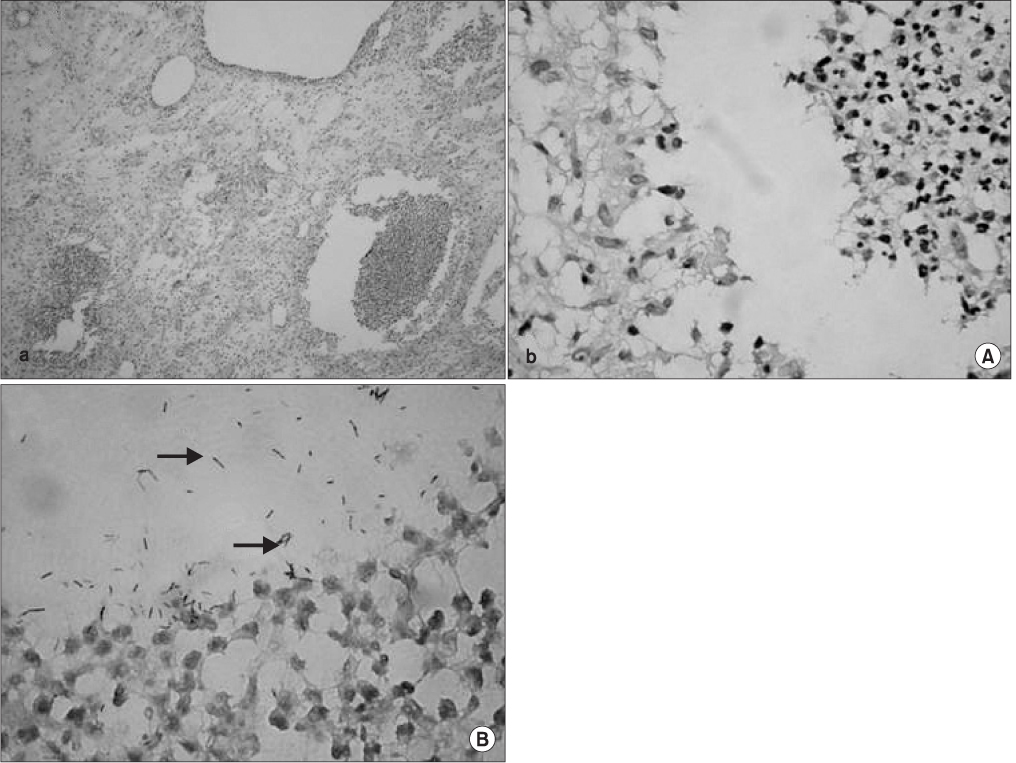
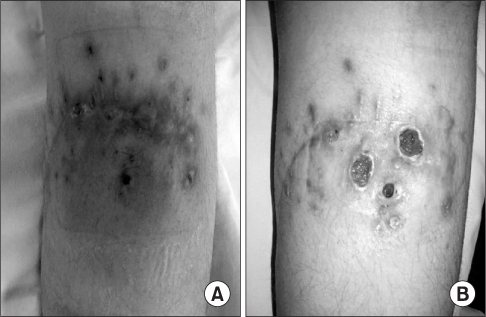
- Chronic granulomatous infection of the skin and soft tissue by nontuberculous mycobacteria in patients with normal immune system is rarely reported. This case was about a child patient, with normal immune system, whose lower leg was lacerated after a slip down in the Philippines and it was previously treated at a hospital in the Philippines. After a couple of surgical debridement of the wound, the cause of the soft tissue infection was found to be a combined infection of nontuberculous mycobacteria and mycobacterium tuberculosis. We present a case that has been rare in Korea, but common overseas.
Keyword
MeSH Terms
Figure
Reference
-
1. Choi YJ, Lee HJ, Lee KY, Ryu DJ, Lee MG. A case of mycobacterium fortuitum infection at the site of acupuncture. Korean J Dermatol. 2009. 47:755–758.2. Liao CH, Lai CC, Ding LW, et al. Skin and soft tissue infection caused by non-tuberculous mycobacteria. Int J Tuberc Lung Dis. 2007. 11:96–102.3. Chen HY, Chen CY, Huang CT, et al. Skin and soft-tissue infection caused by non-tuberculous mycobacteria in Taiwan, 1997-2008. Epidemiol Infect. 2011. 139:121–129.
Article4. Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous mycobacterial pulmonary diseases: a Korean perspective. J Korean Med Sci. 2005. 20:913–925.
Article5. Goodhart GL. Mycobacterium fortuitum osteomyelitis following trauma. J Orthop Trauma. 1993. 7:142–145.
Article6. Devi DR, Indumathi VA, Indira S, Babu PR, Sridharan D, Belwadi MR. Injection site abscess due to Mycobacterium fortuitum: a case report. Indian J Med Microbiol. 2003. 21:133–134.7. Kim BJ, Lee KH, Park BN, et al. Differentiation of mycobacterial species by PCR-restriction analysis of DNA (342 base pairs) of the RNA polymerase gene (rpoB). J Clin Microbiol. 2001. 39:2102–2109.8. Brown-Elliott BA, Wallace RJ Jr. Clinical and taxonomic status of pathogenic nonpigmented or late-pigmenting rapidly growing mycobacteria. Clin Microbiol Rev. 2002. 15:716–746.
Article9. Lee WJ, Kang SM, Sung H, et al. Non-tuberculous mycobacterial infections of the skin: a retrospective study of 29 cases. J Dermatol. 2010. 37:965–972.
Article10. Rotman DA, Blauvelt A, Kerdel FA. Widespread primary cutaneous infection with Mycobacterium fortuitum. Int J Dermatol. 1993. 32:512–514.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Reverse Sural Artery Flap for Soft Tissue Defect of Foot and Ankle in Diabetic Patient
- Intrapelvic Granulomatous Mass Causing Ipsilateral Lower Leg Swelling following Total Hip Arthroplasty: A Case Report
- Reconstruction of a Traumatic Soft Tissue Defect
- The Distally Based Superficial Sural Artery Flap
- A Case of Liposarcoma