J Korean Orthop Assoc.
2012 Dec;47(6):416-424. 10.4055/jkoa.2012.47.6.416.
Perioperative Safety and Efficacy of Multilevel Minimally Invasive Transforaminal Lumbar Interbody Fusion: Comparison with Conventional Open Surgery
- Affiliations
-
- 1Department of Orthopaedic Surgery, Dankook University Hospital, Dankook University Medical College, Cheonan, Korea. osmin71@naver.com
- 2Department of Preventive Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2185304
- DOI: http://doi.org/10.4055/jkoa.2012.47.6.416
Abstract
- PURPOSE
This study was aimed to examine the ways to reduce bleeding through minimally invasive multi-segmental fusion by comparing the results of minimally invasive transforaminal lumbar interbody fusion versus those of conventional posterior interbody fusion depending on the number of fused segment. Moreover, the study identified how the new method of fusion contributed to reducing postoperative complications and to fast recovery.
MATERIALS AND METHODS
This is a retrospective study conducted on 367 spinal stenosis patients who had been followed up for at least one year (170 patients underwent minimally invasive transforaminal lumbar interbody fusion and 197 patients underwent conventional posterior interbody fusion). The study examined blood loss volume, postoperative drainage volume, operation time, visual analogue scale score, pre- and post-operative levels of protein and albumin, as well as postoperative bed rest period between the two groups. Moreover, the study analyzed the presence of complications during the peri-operative period.
RESULTS
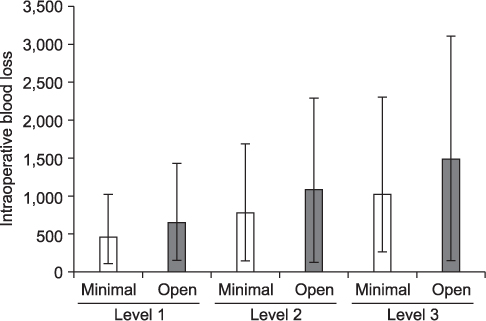
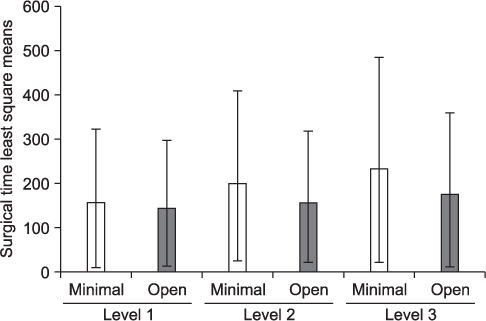
The minimally invasive fusion group exhibited a statistically significant decrease in intraoperative bleeding than the conventional infusion group when the number of fused segments in each group was compared. In addition, the difference in the two groups showed a statistically significant increase as the numbers of fused segments rose (p<0.05). On the other hand, a statistically significant increase was shown in the operation time between the minimally invasive fusion group and the conventional fusion group. The difference in the two groups showed a statistically significant increase as the distance of fused segments was extended (p<0.05).
CONCLUSION
Minimally invasive transforaminal lumbar interbody fusion is thought to be a useful surgical method to minimize bleeding when the limitations of minimal invasive fusion are supplemented by shortening the operation time.
MeSH Terms
Figure
Reference
-
1. Steffee AD, Sitkowski DJ. Posterior lumbar interbody fusion and plates. Clin Orthop Relat Res. 1988. 227:99–102.
Article2. McLaughlin MR, Haid RW Jr, Rodts GE Jr, Subach BR. Posterior lumbar interbody fusion: indications, techniques, and results. Clin Neurosurg. 2000. 47:514–527.3. Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine (Phila Pa 1976). 1997. 22:210–219.4. Deyo RA, Cherkin DC, Loeser JD, Bigos SJ, Ciol MA. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992. 74:536–543.
Article5. Katz JN, Lipson SJ, Brick GW, et al. Clinical correlates of patient satisfaction after laminectomy for degenerative lumbar spinal stenosis. Spine (Phila Pa 1976). 1995. 20:1155–1160.
Article6. Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976). 2003. 28:15 Suppl. S26–S35.
Article7. Cho KJ, Park SR, Jung JH, Park JH. Revision surgery for spinal stenosis developed at the adjacent segment after lumbar fusion. J Korean Orthop Assoc . 2011. 46:205–211.
Article8. Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus. 2006. 20:E6.
Article9. Guiot BH, Khoo LT, Fessler RG. A minimally invasive technique for decompression of the lumbar spine. Spine (Phila Pa 1976). 2002. 27:432–438.
Article10. Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: preliminary clinical results. J Neurosurg. 2002. 97:1 Suppl. 7–12.
Article11. Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. Clin Neurosurg. 2002. 49:499–517.
Article12. Khoo LT, Palmer S, Laich DT, Fessler RG. Minimally invasive percutaneous posterior lumbar interbody fusion. Neurosurgery. 2002. 51:5 Suppl. S166–S161.
Article13. Bagan B, Patel N, Deutsch H, et al. Perioperative complications of minimally invasive surgery (MIS): comparison of MIS and open interbody fusion techniques. Surg Technol Int. 2008. 17:281–286.
Article14. Villavicencio AT, Burneikiene S, Roeca CM, Nelson EL, Mason A. Minimally invasive versus open transforaminal lumbar interbody fusion. Surg Neurol Int. 2010. 1:12.
Article15. Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, Bünger CE. 1997 Volvo Award winner in clinical clinical study. Spine (Phila Pa 1976). 1997. 22:2813–2822.
Article16. Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003. 85:2089–2092.
Article17. Park Y, Ha JW, Sung SY, Oh HC, Yoo JH, Lee YT. Minimally invasive posterior lumbar interbody fusion: comparison with traditional open surgery. J Korean Orthop Assoc. 2006. 41:288–296.
Article18. Cho KJ, Suk SI, Park SR, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2007. 32:2232–2237.
Article19. Park HJ, Lee PE, Lee DK, Park HK. Postoperative complications in patients over 65 years of age with lumbar spinal stenosis and its influencing factors. J Korean Soc Spine Surg. 2006. 13:114–119.
Article20. Furuno KJ, Goldberg AL. The activation of protein degradation in muscle by Ca2+ or muscle injury does not involve a lysosomal mechanism. Biochem J. 1986. 237:859–864.21. Ruberg RL. Role of nutrition in wound healing. Surg Clin North Am. 1984. 64:705–714.22. Haydock DA, Flint MH, Hyde KF, Reilly HC, Poole CA, Hill GL. The efficacy of subcutaneous goretex implants in monitoring wound healing response in experimental protein deficiency. Connect Tissue Res. 1988. 17:159–169.23. Cole CD, McCall TD, Schmidt MH, Dailey AT. Comparison of low back fusion techniques: transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody fusion (PLIF) approaches. Curr Rev Musculoskelet Med. 2009. 2:118–126.24. Deyo RA, Ciol MA, Cherkin DC, Loeser JD, Bigos SJ. Lumbar spinal fusion A cohort study of complications, reoperations, and resource use in the Medicare population. Spine (Phila Pa 1976). 1993. 18:1463–1470.25. Jönsson B, Strömqvist B. Lumbar spine surgery in the elderly. Complications and surgical results. Spine (Phila Pa 1976). 1994. 19:1431–1435.26. Min SH, Lee DH. Minimally invasive transforaminal lumbar interbody fusion in patients with low grade spondylolisthesis: comparison of the unilateral and bilateral approaches. J Korean Orthop Assoc. 2009. 44:429–435.27. Min SH, Hwang SS. Minimal invasive unilateral transforaminal lumbar interbody fusion by sublaminar decompression: comparison to bilateral approach. J Korean Orthop Assoc. 2009. 44:76–82.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Strategy for Uniportal Full-Endoscopic Transforaminal Lumbar Interbody Fusion Using a Large Cage Utilized in Oblique Lumbar Interbody Fusion
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Percutaneous Instrumentation: A Technical Note
- Biportal Endoscopic Transforaminal Interbody Fusion for Lumbar Adjacent Segment Disease: An Illustrative Case and Literature Review
- Radiographic Results of Minimally Invasive (MIS) Lumbar Interbody Fusion (LIF) Compared with Conventional Lumbar Interbody Fusion