J Clin Neurol.
2015 Oct;11(4):339-348. 10.3988/jcn.2015.11.4.339.
Prognostic Tools for Early Mortality in Hemorrhagic Stroke: Systematic Review and Meta-Analysis
- Affiliations
-
- 1Health Evidence Synthesis Group, Norwich Medical School, University of East Anglia, Norwich Research Park, Norwich, UK. y.loke@uea.ac.uk
- 2Institute of Cardiovascular Sciences, University of Manchester, Manchester, UK.
- 3Department of Elderly Medicine, Southend University Hospital Trust, Westcliff-on-Sea, Essex, UK.
- 4Epidemiology Group, Institute of Applied Health Sciences, School of Medicine & Dentistry, University of Aberdeen, Aberdeen, Scotland, UK.
- KMID: 2179753
- DOI: http://doi.org/10.3988/jcn.2015.11.4.339
Abstract
- BACKGROUND AND PURPOSE
Several risk scores have been developed to predict mortality in intracerebral hemorrhage (ICH). We aimed to systematically determine the performance of published prognostic tools.
METHODS
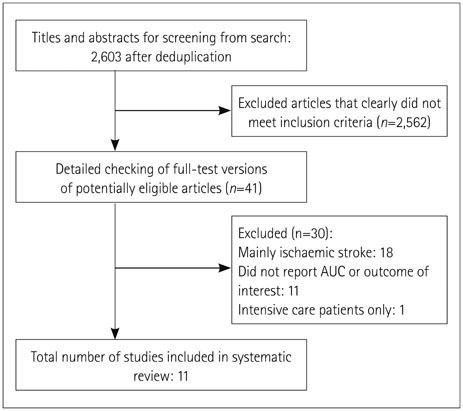
We searched MEDLINE and EMBASE for prognostic models (published between 2004 and April 2014) used in predicting early mortality (<6 months) after ICH. We evaluated the discrimination performance of the tools through a random-effects meta-analysis of the area under the receiver operating characteristic curve (AUC) or c-statistic. We evaluated the following components of the study validity: study design, collection of prognostic variables, treatment pathways, and missing data.
RESULTS
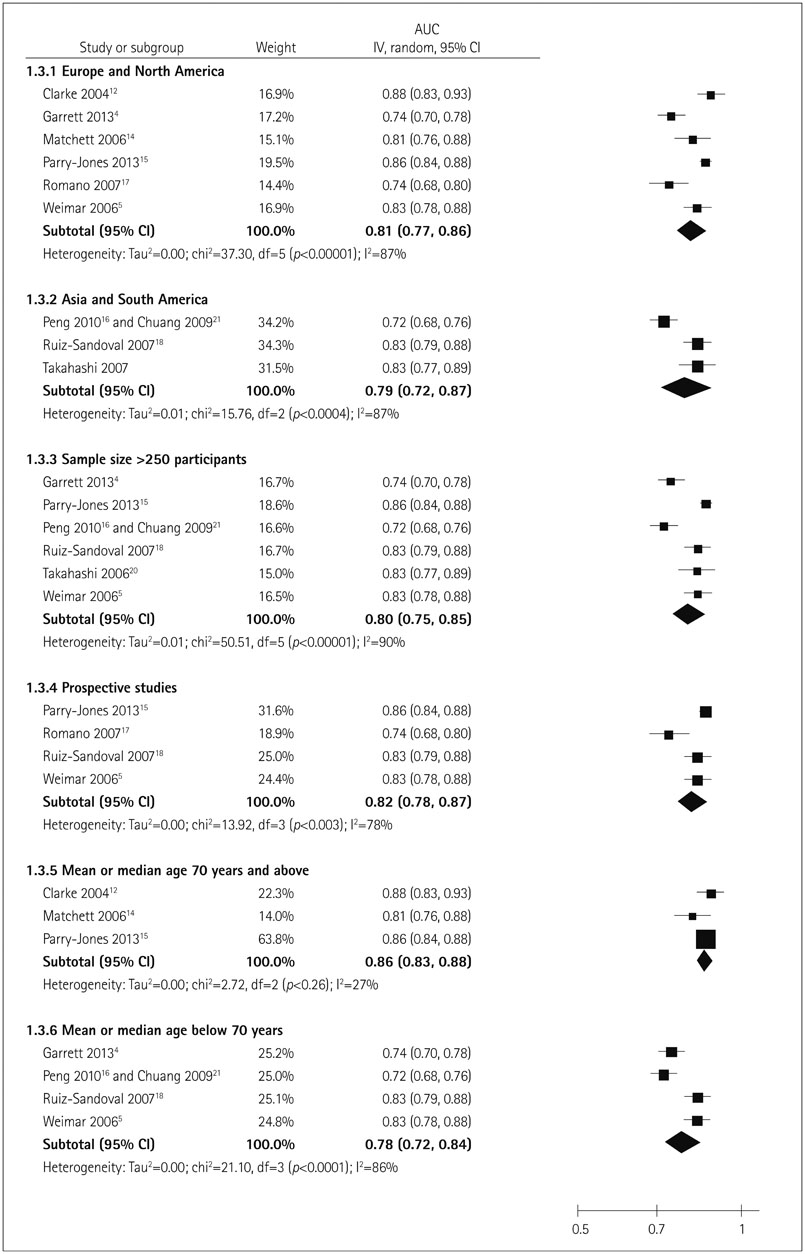
We identified 11 articles (involving 41,555 patients) reporting on the accuracy of 12 different tools for predicting mortality in ICH. Most studies were either retrospective or post-hoc analyses of prospectively collected data; all but one produced validation data. The Hemphill-ICH score had the largest number of validation cohorts (9 studies involving 3,819 patients) within our systematic review and showed good performance in 4 countries, with a pooled AUC of 0.80 [95% confidence interval (CI)=0.77-0.85]. We identified several modified versions of the Hemphill-ICH score, with the ICH-Grading Scale (GS) score appearing to be the most promising variant, with a pooled AUC across four studies of 0.87 (95% CI=0.84-0.90). Subgroup testing found statistically significant differences between the AUCs obtained in studies involving Hemphill-ICH and ICH-GS scores (p=0.01).
CONCLUSIONS
Our meta-analysis evaluated the performance of 12 ICH prognostic tools and found greater supporting evidence for 2 models (Hemphill-ICH and ICH-GS), with generally good performance overall.
Keyword
MeSH Terms
Figure
Reference
-
1. Mackay J, Mensah GA. Atlas of heart disease and stroke. 15 Global burden of stroke [Internet]. Geneva: World Health Organization;2004. cited 2014 Apr 8. Available from: URL: www.who.int/cardiovascular_diseases/en/cvd_atlas_15_burden_stroke.pdf.2. Thrift AG, Dewey HM, Macdonell RA, McNeil JJ, Donnan GA. Incidence of the major stroke subtypes: initial findings from the North East Melbourne stroke incidence study (NEMESIS). Stroke. 2001; 32:1732–1738.3. Krishnamurthi RV, Feigin VL, Forouzanfar MH, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health. 2013; 1:e259–e281.
Article4. Garrett JS, Zarghouni M, Layton KF, Graybeal D, Daoud YA. Validation of clinical prediction scores in patients with primary intracerebral hemorrhage. Neurocrit Care. 2013; 19:329–335.
Article5. Weimar C, Benemann J, Diener HC. German Stroke Study Collaboration. Development and validation of the Essen Intracerebral Haemorrhage Score. J Neurol Neurosurg Psychiatry. 2006; 77:601–605.
Article6. Ariesen MJ, Algra A, van der Worp HB, Rinkel GJ. Applicability and relevance of models that predict short term outcome after intracerebral haemorrhage. J Neurol Neurosurg Psychiatry. 2005; 76:839–844.
Article7. Counsell C, Dennis M. Systematic review of prognostic models in patients with acute stroke. Cerebrovasc Dis. 2001; 12:159–170.
Article8. Agarwal D, Surana A, Chandra S. P-152. Prognostic accuracy of the iCh score on initial evaluation of patients presenting with non-traumatic intracerebral hemorrhage; a systematic review and meta-analysis. Can J Neurol Sci. 2010; 37:3 Suppl 1. S83–S84.9. Austin PC, Steyerberg EW. Interpreting the concordance statistic of a logistic regression model: relation to the variance and odds ratio of a continuous explanatory variable. BMC Med Res Methodol. 2012; 12:82.
Article10. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982; 143:29–36.
Article11. Vellutino FR, Scanlon DM, Zhang H. 14. Identifying reading disability based on response to intervention: evidence from early intervention research. In : Jimerson SR, Burns MK, Van Der Heyden AM, editors. Handbook of response to intervention: the science and practice of assessment and intervention. New York: Springer;2007. p. 194.12. Clarke JL, Johnston SC, Farrant M, Bernstein R, Tong D, Hemphill JC 3rd. External validation of the ICH score. Neurocrit Care. 2004; 1:53–60.
Article13. Li YF, Luo J, Li Q, Jing YJ, Wang RY, Li RS. A new simple model for prediction of hospital mortality in patients with intracerebral hemorrhage. CNS Neurosci Ther. 2012; 18:482–486.
Article14. Matchett SC, Castaldo J, Wasser TE, Baker K, Mathiesen C, Rodgers J. Predicting mortality after intracerebral hemorrhage: comparison of scoring systems and influence of withdrawal of care. J Stroke Cerebrovasc Dis. 2006; 15:144–150.
Article15. Parry-Jones AR, Abid KA, Di Napoli M, Smith CJ, Vail A, Patel HC, et al. Accuracy and clinical usefulness of intracerebral hemorrhage grading scores: a direct comparison in a UK population. Stroke. 2013; 44:1840–1845.
Article16. Peng SY, Chuang YC, Kang TW, Tseng KH. Random forest can predict 30-day mortality of spontaneous intracerebral hemorrhage with remarkable discrimination. Eur J Neurol. 2010; 17:945–950.
Article17. Romano LM, Ioli P, Gonorazky S. Predicting mortality and externally validation of the original intracerebral haemorrhage score after spontaneous intracerebral haemorrhage. Revista Neurológica Argentina. 2007; 32:94–99.18. Ruiz-Sandoval JL, Chiquete E, Romero-Vargas S, Padilla-Martínez JJ, González-Cornejo S. Grading scale for prediction of outcome in primary intracerebral hemorrhages. Stroke. 2007; 38:1641–1644.
Article19. Smith EE, Shobha N, Dai D, Olson DM, Reeves MJ, Saver JL, et al. A risk score for in-hospital death in patients admitted with ischemic or hemorrhagic stroke. J Am Heart Assoc. 2013; 2:e005207.
Article20. Takahashi O, Cook EF, Nakamura T, Saito J, Ikawa F, Fukui T. Risk stratification for in-hospital mortality in spontaneous intracerebral haemorrhage: a Classification and Regression Tree analysis. QJM. 2006; 99:743–750.
Article21. Chuang YC, Chen YM, Peng SK, Peng SY. Risk stratification for predicting 30-day mortality of intracerebral hemorrhage. Int J Qual Health Care. 2009; 21:441–447.
Article22. Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC. The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001; 32:891–897.23. Bushnell CD, Johnston DC, Goldstein LB. Retrospective assessment of initial stroke severity: comparison of the NIH Stroke Scale and the Canadian Neurological Scale. Stroke. 2001; 32:656–660.
Article24. Perry JJ, Goindi R, Brehaut J, Taljaard M, Schneider S, Stiell IG. Emergency physicians' management of transient ischemic attack and desired sensitivity of a clinical decision rule for stroke in three countries. CJEM. 2011; 13:19–27.
Article