J Clin Neurol.
2014 Jul;10(3):197-202. 10.3988/jcn.2014.10.3.197.
T2 Relaxometry Using 3.0-Tesla Magnetic Resonance Imaging of the Brain in Early- and Late-Onset Restless Legs Syndrome
- Affiliations
-
- 1Department of Neurology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea. neurocho@gmail.com
- 2Department of Molecular Medicine, Kyungpook National University Hospital, Daegu, Korea.
- 3Department of Medical & Biological Engineering, Kyungpook National University Hospital, Daegu, Korea.
- 4Department of Radiology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- 5Department of Biomedical Engineering, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 2179445
- DOI: http://doi.org/10.3988/jcn.2014.10.3.197
Abstract
- BACKGROUND AND PURPOSE
Previous T2 relaxometry studies have provided evidence for regional brain iron deficiency in patients with restless legs syndrome (RLS). Measurement of the iron content in several brain regions, and in particular the substantia nigra (SN), in early- and late-onset RLS patients using T2 relaxometry have yielded inconsistent results. In this study the regional iron content was assessed in patients with early- and late-onset RLS using magnetic resonance imaging (MRI), and compared the results with those in controls.
METHODS
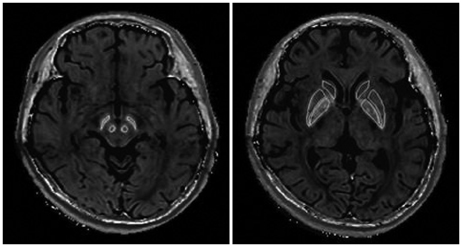
Thirty-seven patients with idiopathic RLS (20 with early onset and 17 with late onset) and 40 control subjects were studied using a 3.0-tesla MRI with a gradient-echo sampling of free induction decay and echo pulse sequence. The regions of interest in the brain were measured independently by two trained analysts using software known as medical image processing, analysis, and visualization. The results were compared and a correlation analysis was conducted to investigate which brain areas were related to RLS clinical variables.
RESULTS
The iron index in the SN was significantly lower in patients with late-onset RLS than in controls (p=0.034), while in patients with early-onset RLS there was no significant difference. There was no significant correlation between the SN iron index of the late-onset RLS group and clinical variables such as disease severity.
CONCLUSIONS
Late-onset RLS is associated with decreased iron content in the SN. This finding supports the hypothesis that regional brain iron deficiency plays a role in the pathophysiology of late-onset RLS.
MeSH Terms
Figure
Reference
-
1. Connor JR. Pathophysiology of restless legs syndrome: evidence for iron involvement. Curr Neurol Neurosci Rep. 2008; 8:162–166.
Article2. Mizuno S, Mihara T, Miyaoka T, Inagaki T, Horiguchi J. CSF iron, ferritin and transferrin levels in restless legs syndrome. J Sleep Res. 2005; 14:43–47.
Article3. Earley CJ, Connor JR, Beard JL, Malecki EA, Epstein DK, Allen RP. Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology. 2000; 54:1698–1700.
Article4. Earley CJ, Connor JR, Beard JL, Clardy SL, Allen RP. Ferritin levels in the cerebrospinal fluid and restless legs syndrome: effects of different clinical phenotypes. Sleep. 2005; 28:1069–1075.
Article5. Godau J, Schweitzer KJ, Liepelt I, Gerloff C, Berg D. Substantia nigra hypoechogenicity: definition and findings in restless legs syndrome. Mov Disord. 2007; 22:187–192.
Article6. Connor JR, Boyer PJ, Menzies SL, Dellinger B, Allen RP, Ondo WG, et al. Neuropathological examination suggests impaired brain iron acquisition in restless legs syndrome. Neurology. 2003; 61:304–309.
Article7. Connor JR, Wang XS, Patton SM, Menzies SL, Troncoso JC, Earley CJ, et al. Decreased transferrin receptor expression by neuromelanin cells in restless legs syndrome. Neurology. 2004; 62:1563–1567.
Article8. Brass SD, Chen NK, Mulkern RV, Bakshi R. Magnetic resonance imaging of iron deposition in neurological disorders. Top Magn Reson Imaging. 2006; 17:31–40.
Article9. Kosta P, Argyropoulou MI, Markoula S, Konitsiotis S. MRI evaluation of the basal ganglia size and iron content in patients with Parkinson's disease. J Neurol. 2006; 253:26–32.
Article10. Argyropoulou MI, Astrakas L. MRI evaluation of tissue iron burden in patients with beta-thalassaemia major. Pediatr Radiol. 2007; 37:1191–1200. quiz 1308-1309.
Article11. Allen RP, Barker PB, Wehrl F, Song HK, Earley CJ. MRI measurement of brain iron in patients with restless legs syndrome. Neurology. 2001; 56:263–265.
Article12. Earley CJ, Barker PB, Horská A, Allen RP. MRI-determined regional brain iron concentrations in early- and late-onset restless legs syndrome. Sleep Med. 2006; 7:458–461.
Article13. Godau J, Klose U, Di Santo A, Schweitzer K, Berg D. Multiregional brain iron deficiency in restless legs syndrome. Mov Disord. 2008; 23:1184–1187.
Article14. Astrakas LG, Konitsiotis S, Margariti P, Tsouli S, Tzarouhi L, Argyropoulou MI. T2 relaxometry and fMRI of the brain in late-onset restless legs syndrome. Neurology. 2008; 71:911–916.
Article15. Knake S, Heverhagen JT, Menzler K, Keil B, Oertel WH, Stiasny-Kolster K. Normal regional brain iron concentration in restless legs syndrome measured by MRI. Nat Sci Sleep. 2009; 2:19–22.
Article16. Margariti PN, Astrakas LG, Tsouli SG, Hadjigeorgiou GM, Konitsiotis S, Argyropoulou MI. Investigation of unmedicated early onset restless legs syndrome by voxel-based morphometry, T2 relaxometry, and functional MR imaging during the night-time hours. AJNR Am J Neuroradiol. 2012; 33:667–672.
Article17. Gelman N, Gorell JM, Barker PB, Savage RM, Spickler EM, Windham JP, et al. MR imaging of human brain at 3.0 T: preliminary report on transverse relaxation rates and relation to estimated iron content. Radiology. 1999; 210:759–767.
Article18. Cho YW, Shin WC, Yun CH, Hong SB, Kim JH, Allen RP, et al. Epidemiology of restless legs syndrome in Korean adults. Sleep. 2008; 31:219–223.
Article19. Hening WA, Allen RP, Washburn M, Lesage S, Earley CJ. Validation of the Hopkins telephone diagnostic interview for restless legs syndrome. Sleep Med. 2008; 9:283–289.
Article20. Cho YW, Lee MY, Yun CH, Shin WC, Hong SB, Kim JH. The reliability and validity of the Korean version of paradigm of questions for epidemiology studies of restless legs syndrome and the Johns Hopkins telephone diagnostic interview form for the restless legs syndrome. J Korean Neurol Assoc. 2007; 25:494–499.21. Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath. 2011; 15:377–384.
Article22. Sohn SI, Kim do H, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012; 16:803–812.
Article23. Yang JG, Kim DH, Lee JH, Park KH, Jung KY, Shin WC, et al. The reliability and validity of the Korean versions of the International Restless Legs Scale and the Restless Legs Syndrome Quality of Life Questionnaire. J Korean Neurol Assoc. 2010; 28:263–269.24. Walters AS, LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP, et al. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003; 4:121–132.
Article25. Aguirre P, Urrutia P, Tapia V, Villa M, Paris I, Segura-Aguilar J, et al. The dopamine metabolite aminochrome inhibits mitochondrial complex I and modifies the expression of iron transporters DMT1 and FPN1. Biometals. 2012; 25:795–803.
Article26. de La Fuente-Fernández R, Lim AS, Sossi V, Holden JE, Calne DB, Ruth TJ, Stoessl AJ. Apomorphine-induced changes in synaptic dopamine levels: positron emission tomography evidence for presynaptic inhibition. J Cereb Blood Flow Metab. 2001; 21:1151–1159.
Article27. Ordidge RJ, Gorell JM, Deniau JC, Knight RA, Helpern JA. Assessment of relative brain iron concentrations using T2-weighted and T2*-weighted MRI at 3 Tesla. Magn Reson Med. 1994; 32:335–341.
Article28. Gorell JM, Ordidge RJ, Brown GG, Deniau JC, Buderer NM, Helpern JA. Increased iron-related MRI contrast in the substantia nigra in Parkinson's disease. Neurology. 1995; 45:1138–1143.
Article29. Oikawa H, Sasaki M, Tamakawa Y, Ehara S, Tohyama K. The substantia nigra in Parkinson disease: proton density-weighted spin-echo and fast short inversion time inversion-recovery MR findings. AJNR Am J Neuroradiol. 2002; 23:1747–1756.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Introduction for the Questionnaires for Restless Legs Syndrome
- A Case of Idiopathic Restless Legs Syndrome in a Child
- Unilateral Restless Legs Syndrome
- Signal Hyperintensities on Brain Magnetic Resonance Imaging in Late-life Depressive Patients
- Restless Legs Syndrome: An Update in Diagnosis and Management