J Clin Neurol.
2011 Dec;7(4):223-226. 10.3988/jcn.2011.7.4.223.
Leukoencephalopathy and Akinetic Mutism in a Married Couple: A Probable Association with Oriental Medicine
- Affiliations
-
- 1Department of Neurology, College of Medicine, The Catholic University of Korea, Seoul, Korea. neuronet@catholic.ac.kr
- KMID: 2179008
- DOI: http://doi.org/10.3988/jcn.2011.7.4.223
Abstract
- BACKGROUND
Oriental medicines have been associated with severe psychiatric, neurological, and other adverse medical events. These medicines occasionally cause a typical reversible toxic encephalopathy, but most such cases are not recognized because these adverse events are complex and are associated with other systemic signs and symptoms.
CASE REPORT
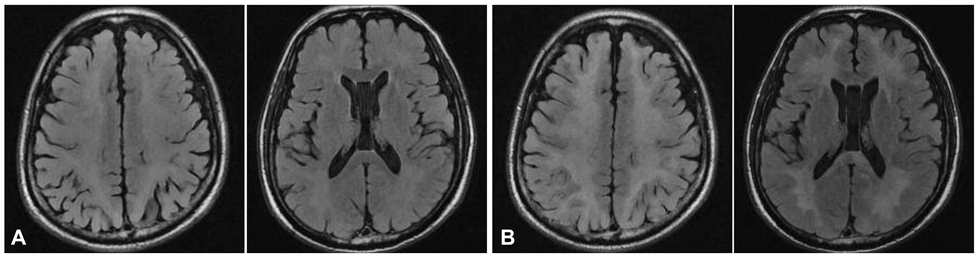
We describe a married couple with rapid progressive cognitive impairment and akinetic mutism after taking the same oriental medicines on the same day. Brain magnetic resonance images of the couple showed typical leukoencephalopathy in the periventricular white matter and basal ganglia regions, bilaterally.
CONCLUSIONS
The development of neurobehavioral symptoms and toxic leukoencephalopathy in both patients following the ingestion of oriental medicines is suggestive of a cause-and-effect association, although such a relationship needs to be verified.
MeSH Terms
Figure
Reference
-
1. Filley CM, Kleinschmidt-DeMasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001. 345:425–432.
Article2. Jung KH, Chu K, Kim YA, Jeon BS. Rapidly progressive toxic leukoencephalomyelopathy with myelodysplastic syndrome: a clinicopathological correlation. J Clin Neurol. 2007. 3:45–49.
Article3. Ernst E. Serious psychiatric and neurological adverse effects of herbal medicines -- a systematic review. Acta Psychiatr Scand. 2003. 108:83–91.
Article4. Rella J, Marcus S, Wagner BJ. Rapid cyanide detection using the Cyantesmo kit. J Toxicol Clin Toxicol. 2004. 42:897–900.
Article5. McKinney AM, Kieffer SA, Paylor RT, SantaCruz KS, Kendi A, Lucato L. Acute toxic leukoencephalopathy: potential for reversibility clinically and on MRI with diffusion-weighted and FLAIR imaging. AJR Am J Roentgenol. 2009. 193:192–206.
Article6. Nam TS, Choi SM, Kang KW, Kim JT, Lee SH, Park MS, et al. Acute toxic encephalopathy due to the ingestion of Rhus extract. J Clin Neurosci. 2009. 16:1377–1378.
Article7. Kim JS, Chung SW, Chung TI, Park JW, Lee KS, Lee JH. Posterior reversible leukoencephalopathy syndrome: possible relation to licorice. Eur J Radiol Extra. 2003. 46:83–85.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Leukoencephalopathy and Akinetic Mutism in a Married Couple: A Probable Association with Oriental Medicine
- The Effect of Levodopa on Akinetic Mutism in Bilateral Anterior Cerebral Artery Infarction: A case report
- A Case of Akinetic Mutism Caused by Volume Change of Cerebral Ventricles
- Two Cases of Reversible Leukoencephalopathy, Caused by 5-Fluorouracil, Presenting as Akinetic Mutism
- Transient Akinetic Mutism Following General Anesthesia: A case report