J Cardiovasc Ultrasound.
2012 Dec;20(4):174-180. 10.4250/jcu.2012.20.4.174.
The Association of Left Ventricular Hypertrophy with Intraventricular Dyssynchrony at Rest and during Exercise in Hypertensive Patients
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Soonchunhyang University Hospital, Bucheon, Korea. haesunfree@hotmail.com
- 2Department of Rehabilitation Medicine, Gachon University Gil Hospital, Incheon, Korea.
- KMID: 2177404
- DOI: http://doi.org/10.4250/jcu.2012.20.4.174
Abstract
- BACKGROUND
Impaired exercise tolerance with dyspnea is common in hypertensive patients and this may be due to the exaggeration of nonuniform ventricular activation during exercise. So we want to evaluate the effect of left ventricular hypertrophy (LVH) on systolic intraventricular dyssynchrony during exercise.
METHODS
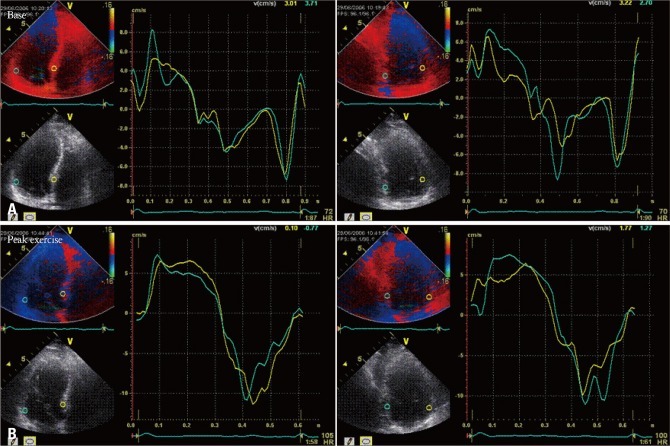
A total of 85 patients with hypertension who having exertional dyspnea and 30 control individuals were enrolled. Exercise stress echocardiography was performed using a symptom limited, multistage supine bicycle test. To evaluate the dyssynchrony of left ventricular (LV), we calculated the standard deviation (SD) of the averaged time-to-peak systolic velocity (TPs-SD, ms) of 12 middle and basal LV segments obtained from the three standard apical views at rest and peak exercise.
RESULTS
There was no significant difference in systolic blood pressure (BP) and heart rate between the two groups. TPs-SD was significantly higher in patients with LVH at rest (31.5 +/- 12.1 vs. 22.0 +/- 12.6 ms, p = 0.002) with exaggeration of the degree at peak exercise (39.0 +/- 11.9 vs. 24.6 +/- 13.3 ms, p < 0.001). Multiple regression analysis showed LV mass index was independently associated with LV dyssynchrony at peak exercise (beta = 0.515, p = 0.001) when controlled for age, sex, and systolic BP at peak exercise.
CONCLUSION
Intraventricular systolic dyssynchrony during exercise is significantly associated with the degree of LVH in hypertensive patients.
MeSH Terms
Figure
Cited by 1 articles
-
Is Dynamic Left Ventricular Dyssynchrony a Novel Surrogate Marker in the Patient with Hypertension?
Wook-Jin Chung
J Cardiovasc Ultrasound. 2012;20(4):172-173. doi: 10.4250/jcu.2012.20.4.172.
Reference
-
1. Grossman W, Jones D, McLaurin LP. Wall stress and patterns of hypertrophy in the human left ventricle. J Clin Invest. 1975; 56:56–64. PMID: 124746.2. Goodwin JF. Congestive and hypertrophic cardiomyopathies. A decade of study. Lancet. 1970; 1:732–739. PMID: 4191245.3. Yelamarty RV, Moore RL, Yu FT, Elensky M, Semanchick AM, Cheung JY. Relaxation abnormalities in single cardiac myocytes from renovascular hypertensive rats. Am J Physiol. 1992; 262(4 Pt 1):C980–C990. PMID: 1533096.4. Hess OM, Schneider J, Koch R, Bamert C, Grimm J, Krayenbuehl HP. Diastolic function and myocardial structure in patients with myocardial hypertrophy. Special reference to normalized viscoelastic data. Circulation. 1981; 63:360–371. PMID: 6450003.5. Shapiro LM, McKenna WJ. Left ventricular hypertrophy. Relation of structure to diastolic function in hypertension. Br Heart J. 1984; 51:637–642. PMID: 6234010.6. Douglas PS, Tallant B. Hypertrophy, fibrosis and diastolic dysfunction in early canine experimental hypertension. J Am Coll Cardiol. 1991; 17:530–536. PMID: 1825098.7. D'Andrea A, Caso P, Severino S, Scotto di Uccio F, Vigorito F, Ascione L, Scherillo M, Calabrò R. Association between intraventricular myocardial systolic dyssynchrony and ventricular arrhythmias in patients with hypertrophic cardiomyopathy. Echocardiography. 2005; 22:571–578. PMID: 16060893.8. Mishiro Y, Oki T, Iuchi A, Tabata T, Yamada H, Abe M, Onose Y, Ito S, Nishitani H, Harada M, Taoka Y. Regional left ventricular myocardial contraction abnormalities and asynchrony in patients with hypertrophic cardiomyopathy evaluated by magnetic resonance spatial modulation of magnetization myocardial tagging. Jpn Circ J. 1999; 63:442–446. PMID: 10406583.9. Gillebert TC, Lew WY. Nonuniformity and volume loading independently influence isovolumic relaxation rates. Am J Physiol. 1989; 257(6 Pt 2):H1927–H1935. PMID: 2603977.10. Cardim N, Oliveira AG, Longo S, Ferreira T, Pereira A, Reis RP, Correia JM. Doppler tissue imaging: regional myocardial function in hypertrophic cardiomyopathy and in athlete's heart. J Am Soc Echocardiogr. 2003; 16:223–232. PMID: 12618730.11. Abe H, Tomotsune K. Asynchronous relaxation of the ischemic left ventricle. Jpn Circ J. 1982; 46:103–112. PMID: 6976448.12. De Marchi SF, Allemann Y, Seiler C. Relaxation in hypertrophic cardiomyopathy and hypertensive heart disease: relations between hypertrophy and diastolic function. Heart. 2000; 83:678–684. PMID: 10814629.13. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Chamber Quantification Writing Group. American Society of Echocardiography's Guidelines and Standards Committee. European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463. PMID: 16376782.14. Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, Lee MM, Park YB, Choi YS, Seo JD, Lee YW. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol. 1997; 30:474–480. PMID: 9247521.15. Chang SA, Kim HK, Kim DH, Kim YJ, Sohn DW, Oh BH, Park YB. Left ventricular systolic and diastolic dyssynchrony in asymptomatic hypertensive patients. J Am Soc Echocardiogr. 2009; 22:337–342. PMID: 19269134.16. Tan HW, Zheng GL, Li L, Wang ZH, Gong HP, Zhang Y, Zhong M, Zhang W. Impaired left ventricular synchronicity in hypertensive patients with ventricular hypertrophy. J Hypertens. 2008; 26:553–559. PMID: 18300868.17. Ha TH, Seo HS, Choo WJ, Choi J, Suh J, Cho YH, Lee NH. The Effect of Metabolic Syndrome on Myocardial Contractile Reserve during Exercise in Non-Diabetic Hypertensive Subjects. J Cardiovasc Ultrasound. 2011; 19:176–182. PMID: 22259660.18. Kwon BJ, Choi KY, Kim DB, Jang SW, Cho EJ, Youn HJ, Kim JH. Systolic synchrony is impaired in nonleft ventricular hypertrophy of never-treated hypertensive patients. J Hypertens. 2011; 29:2246–2254. PMID: 21918472.19. Nagueh SF. Mechanical dyssynchrony in congestive heart failure: diagnostic and therapeutic implications. J Am Coll Cardiol. 2008; 51:18–22. PMID: 18174031.20. Yuda S, Short L, Leano R, Marwick TH. Myocardial abnormalities in hypertensive patients with normal and abnormal left ventricular filling: a study of ultrasound tissue characterization and strain. Clin Sci (Lond). 2002; 103:283–293. PMID: 12193154.21. Masoudi FA, Havranek EP, Smith G, Fish RH, Steiner JF, Ordin DL, Krumholz HM. Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol. 2003; 41:217–223. PMID: 12535812.22. Lund LH, Mancini D. Heart failure in women. Med Clin North Am. 2004; 88:1321–1345. xiiPMID: 15331319.23. Gottlieb SS, Khatta M, Friedmann E, Einbinder L, Katzen S, Baker B, Marshall J, Minshall S, Robinson S, Fisher ML, Potenza M, Sigler B, Baldwin C, Thomas SA. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol. 2004; 43:1542–1549. PMID: 15120809.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Left Ventricular Hypertrophy on Ventricular Performance in Essential Hypertension
- A Comparative Study of Left Ventricular Diastolic Function between Hypertrophic Cardiomyopathy and Hypertensive Patients with Left Ventricular Hypertrophy
- Left Ventricular Diastolic Functions by M-Mode Echocardiogram in Essential Hypertensive Patients
- Relationship between Exercise-induced Blood Pressure Response and Left Ventricular Hypertrophy in Patients with Hypertension
- Left Ventricular Dyssynchrony in Patients Showing Diastolic Dysfunction without Overt Symptoms of Heart Failure