J Adv Prosthodont.
2013 Nov;5(4):396-401. 10.4047/jap.2013.5.4.396.
In vitro comparison of two different materials for the repair of urethan dimethacrylate denture bases
- Affiliations
-
- 1Department of Prosthodontics, Faculty of Dentistry, Istanbul University, Istanbul, Turkey. geckili@istanbul.edu.tr
- 2Istanbul Technical University, Department of Mechanical Engineering, Istanbul, Turkey.
- KMID: 2176528
- DOI: http://doi.org/10.4047/jap.2013.5.4.396
Abstract
- PURPOSE
The purpose of this in vitro study was to investigate the flexural properties of a recently introduced urethane dimethacrylate denture base material (Eclipse) after being repaired with two different materials.
MATERIALS AND METHODS
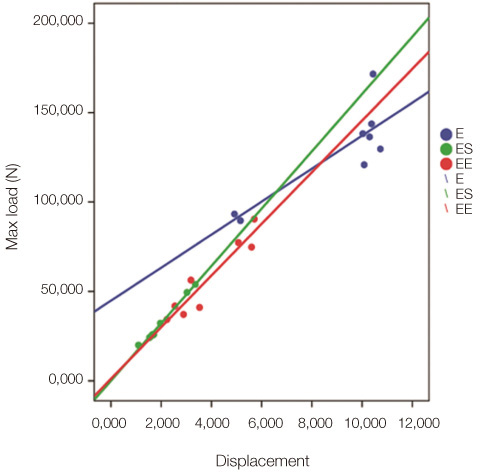
Two repair groups and a control group consisting of 10 specimens each were generated. The ES group was repaired with auto-polymerizing polymer. The EE group was repaired with the Eclipse. The E group was left intact as a control group. A 3-point bending test device which was set to travel at a crosshead speed of 5 mm/min was used. Specimens were loaded until fracture occurred and the mean displacement, maximum load, flexural modulus and flexural strength values and standard deviations were calculated for each group and the data were statistically analyzed. The results were assessed at a significance level of P<.05.
RESULTS
The mean "displacement", "maximum load before fracture", "flexural strength" and "flexural modulus" rates of Group E were statistically significant higher than those of Groups ES and EE, but no significant difference (P>.05) was found between the mean values of Group ES and EE. There was a statistically significant positive relation (P<.01) between the displacement and maximum load of Group ES (99.5%), Group EE (94.3%) and Group E (84.4%).
CONCLUSION
The more economic and commonly used self-curing acrylic resin can be recommended as an alternative repair material for Eclipse denture bases.
Keyword
MeSH Terms
Figure
Reference
-
1. Diwan R. Materials Prescribed in the Management of Edentulous Patients. In : Zarb G, Bolender CL, Eckert SE, editors. Prosthodontic treatment for edentulous Patients: complete dentures and implant-supported prostheses. 12th ed. St. Louis: CV. Mosby;2004. p. 190–207.2. Meng TR Jr, Latta MA. Physical properties of four acrylic denture base resins. J Contemp Dent Pract. 2005; 6:93–100.3. Murray MD, Darvell BW. The evolution of the complete denture base. Theories of complete denture retention-a review. Part 1. Aust Dent J. 1993; 38:216–219.4. Parvizi A, Lindquist T, Schneider R, Williamson D, Boyer D, Dawson DV. Comparison of the dimensional accuracy of injection-molded denture base materials to that of conventional pressure-pack acrylic resin. J Prosthodont. 2004; 13:83–89.5. Pfeiffer P, Rosenbauer EU. Residual methyl methacrylate monomer, water sorption, and water solubility of hypoallergenic denture base materials. J Prosthet Dent. 2004; 92:72–78.6. Price CA. A history of dental polymers. Aust Prosthodont J. 1994; 8:47–54.7. Dar-Odeh NS, Harrison A, Abu-Hammad O. An evaluation of self-cured and visible light-cured denture base materials when used as a denture base repair material. J Oral Rehabil. 1997; 24:755–760.8. Polyzois GL, Tarantili PA, Frangou MJ, Andreopoulos AG. Fracture force, deflection at fracture, and toughness of repaired denture resin subjected to microwave polymerization or reinforced with wire or glass fiber. J Prosthet Dent. 2001; 86:613–619.9. Vallittu PK, Lassila VP, Lappalainen R. Evaluation of damage to removable dentures in two cities in Finland. Acta Odontol Scand. 1993; 51:363–369.10. Beyli MS, von Fraunhofer JA. An analysis of causes of fracture of acrylic resin dentures. J Prosthet Dent. 1981; 46:238–241.11. Darbar UR, Huggett R, Harrison A. Denture fracture-a survey. Br Dent J. 1994; 176:342–345.12. McCabe JF, Carrick TE, Chadwick RG, Walls AW. Alternative approaches to evaluating the fatigue characteristics of materials. Dent Mater. 1990; 6:24–28.13. Diaz-Arnold AM, Vargas MA, Shaull KL, Laffoon JE, Qian F. Flexural and fatigue strengths of denture base resin. J Prosthet Dent. 2008; 100:47–51.14. Rodford RA. Further development and evaluation of high impact strength denture base materials. J Dent. 1990; 18:151–157.15. Rodford RA, Braden M. Further observations on high impact strength denture-base materials. Biomaterials. 1992; 13:726–728.16. Machado C, Sanchez E, Azer SS, Uribe JM. Comparative study of the transverse strength of three denture base materials. J Dent. 2007; 35:930–933.17. Radzi Z, Abu Kasim NH, Yahya NA, Gan SN. Impact strength of an experimental polyurethane-based polymer. Annal Dent Univ Malaya. 2007; 14:46–51.18. Machado AL, Puckett AD, Breeding LC, Wady AF, Vergani CE. Effect of thermocycling on the flexural and impact strength of urethane-based and high-impact denture base resins. Gerodontology. 2012; 29:e318–e323.19. Andreopoulos AG, Polyzois GL. Repair of denture base resins using visible light-cured materials. J Prosthet Dent. 1994; 72:462–468.20. Thean HP, Chew CL, Goh KI, Norman RD. An evaluation of bond strengths of denture repair resins by a torsional method. Aust Dent J. 1998; 43:5–8.21. Beyli MS, von Fraunhofer JA. Repair of fractured acrylic resin. J Prosthet Dent. 1980; 44:497–503.22. Ward JE, Moon PC, Levine RA, Behrendt CL. Effect of repair surface design, repair material, and processing method on the transverse strength of repaired acrylic denture resin. J Prosthet Dent. 1992; 67:815–820.23. Vallittu PK, Lassila VP, Lappalainen R. Wetting the repair surface with methyl methacrylate affects the transverse strength of repaired heat-polymerized resin. J Prosthet Dent. 1994; 72:639–643.24. Zappini G, Kammann A, Wachter W. Comparison of fracture tests of denture base materials. J Prosthet Dent. 2003; 90:578–585.25. Uzun G, Hersek N. Comparison of the fracture resistance of six denture base acrylic resins. J Biomater Appl. 2002; 17:19–29.26. Phoenix RD, Mansueto MA, Ackerman NA, Jones RE. Evaluation of mechanical and thermal properties of commonly used denture base resins. J Prosthodont. 2004; 13:17–27.27. Tirapelli C, Ravagnani C, Panzeri Fde C, Panzeric H. Fiber-reinforced composites: effect of fiber position, fiber framework, and wetting agent on flexural strength. Int J Prosthodont. 2005; 18:201–202.28. Ogle RE, Sorensen SE, Lewis EA. A new visible light-cured resin system applied to removable prosthodontics. J Prosthet Dent. 1986; 56:497–506.29. Fellman S. Visible light-cured denture base resin used in making dentures with conventional teeth. J Prosthet Dent. 1989; 62:356–359.30. Khan Z, Haeberle CB. One-appointment construction of an immediate transitional complete denture using visible light-cured resin. J Prosthet Dent. 1992; 68:500–502.31. Khan Z, von Fraunhofer JA, Razavi R. The staining characteristics, transverse strength, and microhardness of a visible light-cured denture base material. J Prosthet Dent. 1987; 57:384–386.32. Tan HK, Brudvik JS, Nicholls JI, Smith DE. Adaptation of a visible light-cured denture base material. J Prosthet Dent. 1989; 61:326–331.33. Nishigawa G, Maruo Y, Oka M, Okamoto M, Minagi S, Irie M, Suzuki K. Effect of plasma treatment on adhesion of self-curing repair resin to acrylic denture base. Dent Mater J. 2004; 23:545–549.34. Yunus N, Rashid AA, Azmi LL, Abu-Hassan MI. Some flexural properties of a nylon denture base polymer. J Oral Rehabil. 2005; 32:65–71.35. Hedzelek W, Gajdus P. Comparison of mechanical strength of palatal denture bases made from various plastic materials. Int J Prosthodont. 2006; 19:193–194.36. Nakamura M, Takahashi H, Hayakawa I. Reinforcement of denture base resin with short-rod glass fiber. Dent Mater J. 2007; 26:733–738.37. Gonda T, Maeda Y, Walton JN, MacEntee MI. Fracture incidence in mandibular overdentures retained by one or two implants. J Prosthet Dent. 2010; 103:178–181.38. Pfeiffer P, An N, Schmage P. Repair strength of hypoallergenic denture base materials. J Prosthet Dent. 2008; 100:292–301.39. Kostoulas I, Kavoura VT, Frangou MJ, Polyzois GL. Fracture force, deflection, and toughness of acrylic denture repairs involving glass fiber reinforcement. J Prosthodont. 2008; 17:257–261.40. Faot F, da Silva WJ, da Rosa RS, Del Bel Cury AA, Garcia RC. Strength of denture base resins repaired with auto-and visible light-polymerized materials. J Prosthodont. 2009; 18:496–502.41. Rached RN, Powers JM, Del Bel Cury AA. Repair strength of autopolymerizing, microwave, and conventional heat-polymerized acrylic resins. J Prosthet Dent. 2004; 92:79–82.42. Minami H, Suzuki S, Kurashige H, Minesaki Y, Tanaka T. Flexural strengths of denture base resin repaired with autopolymerizing resin and reinforcements after thermocycle stressing. J Prosthodont. 2005; 14:12–18.43. Johnston EP, Nicholls JI, Smith DE. Flexure fatigue of 10 commonly used denture base resins. J Prosthet Dent. 1981; 46:478–483.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative evaluation of sodium hypochlorite and microwave disinfection on dimensional stability of denture bases
- Adherence of Candida to complete denture surfaces in vitro: A comparison of conventional and CAD/CAM complete dentures
- An in vitro study on cellular response of several denture base resins
- Three dimensional deformation of dry-stored complete denture base at room temperature
- Comparison of polymer-based temporary crown and fixed partial denture materials by diametral tensile strength