J Breast Cancer.
2016 Mar;19(1):68-75. 10.4048/jbc.2016.19.1.68.
Oncologic Safety of Immediate Breast Reconstruction for Invasive Breast Cancer Patients: A Matched Case Control Study
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea. hanw@snu.ac.kr
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Plastic and Reconstructive Surgery, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2176323
- DOI: http://doi.org/10.4048/jbc.2016.19.1.68
Abstract
- PURPOSE
The purpose of this study was to compare locoregional recurrence-free survival (LRFS) and disease-free survival (DFS) between patients undergoing mastectomy and immediate breast reconstruction (IBR) and those undergoing mastectomy alone.
METHODS
A retrospective review of patients who underwent mastectomy and immediate breast reconstruction for resectable invasive breast cancer between 2002 and 2010 at a single center was conducted. These cases were matched to patients who underwent mastectomy alone in the same time period, performed by 1:2 matching. Matching control variables included age, tumor size, axillary lymph node metastasis, and estrogen receptor status. Overall, 189 patients were identified in the IBR group, and 362 patients were matched to this group.
RESULTS
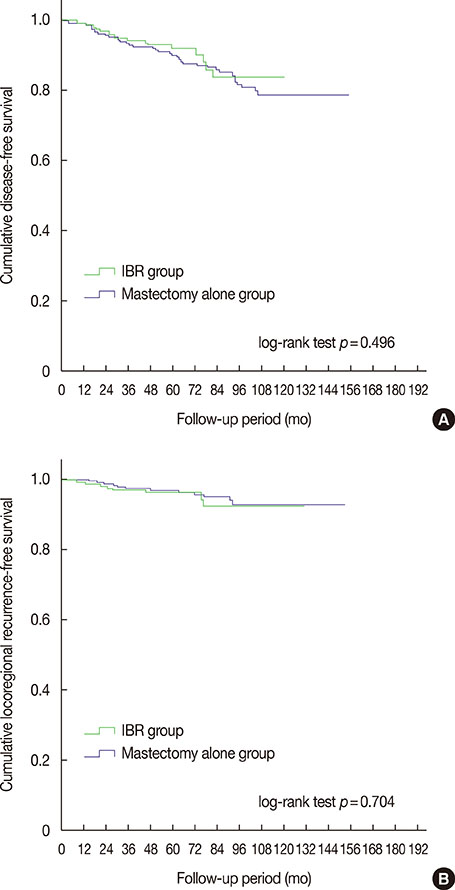
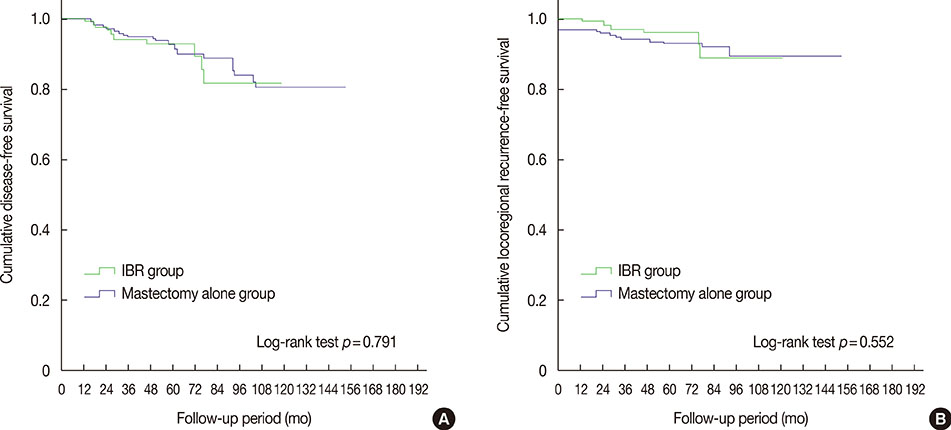
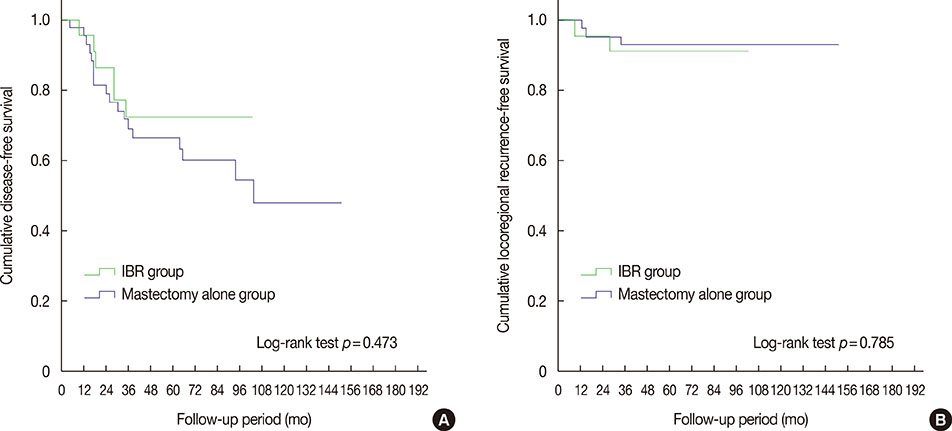
In the IBR group, 75 patients (39.7%) underwent conventional total mastectomy, 78 (41.3%) underwent skin-sparing mastectomy (SSM), and 36 (19.0%) underwent nipple-sparing mastectomy (NSM). The IBR group was significantly younger than the control group (41.9 and 45.1 years, respectively) (p=0.032), in spite of matching between three age groups. The DFS rates were similar between the IBR group and mastectomy alone group, at 92.0% and 89.9%, respectively, at 5-year follow-up (log-rank test, p=0.496). The 5-year LRFS was 96.2% in the IBR group and 96.4% in the mastectomy alone group (log-rank test, p=0.704), similar to data from previous reports. Subgroup analyses for SSM or NSM patients showed no differences in LRFS and DFS between the two groups. Additionally, in stage III patients, IBR did not cause an increase in recurrence.
CONCLUSION
IBR after mastectomy, including both SSM and NSM, had no negative impact on recurrence or patient survival, even in patients with advanced disease.
MeSH Terms
Figure
Cited by 2 articles
-
Oncologic Outcomes after Immediate Breast Reconstruction Following Total Mastectomy in Patients with Breast Cancer: A Matched Case-Control Study
Jai Min Ryu, Hyun-June Paik, Sungmin Park, Ha Woo Yi, Seok Jin Nam, Seok Won Kim, Se Kyung Lee, Jonghan Yu, Soo Youn Bae, Jeong Eon Lee
J Breast Cancer. 2017;20(1):74-81. doi: 10.4048/jbc.2017.20.1.74.Changes in Korean National Healthcare Insurance Policy and Breast Cancer Surgery Trend in Korea
Musaed Rayzah, Jai Min Ryu, Jun-Hee Lee, Seok Jin Nam, Seok Won Kim, Se Kyung Lee, Jonghan Yu, Kyeong-Tae Lee, Sa-Ik Bang, Goo-Hyun Mun, Jai-Kyong Pyon, Byung-Joon Jeon, Jeong Eon Lee
J Korean Med Sci. 2021;36(29):e194. doi: 10.3346/jkms.2021.36.e194.
Reference
-
1. Liang TJ, Wang BW, Liu SI, Yeh MH, Chen YC, Chen JS, et al. Recurrence after skin-sparing mastectomy and immediate transverse rectus abdominis musculocutaneous flap reconstruction for invasive breast cancer. World J Surg Oncol. 2013; 11:194.
Article2. Drucker-Zertuche M, Robles-Vidal C. A 7 year experience with immediate breast reconstruction after skin sparing mastectomy for cancer. Eur J Surg Oncol. 2007; 33:140–146.
Article3. van Mierlo DR, Lopez Penha TR, Schipper RJ, Martens MH, Serroyen J, Lobbes MB, et al. No increase of local recurrence rate in breast cancer patients treated with skin-sparing mastectomy followed by immediate breast reconstruction. Breast. 2013; 22:1166–1170.
Article4. Kim Z, Min SY, Yoon CS, Jung KW, Ko BS, Kang E, et al. The basic facts of Korean breast cancer in 2012: results from a nationwide survey and breast cancer registry database. J Breast Cancer. 2015; 18:103–111.
Article5. Romics L Jr, Chew BK, Weiler-Mithoff E, Doughty JC, Brown IM, Stallard S, et al. Ten-year follow-up of skin-sparing mastectomy followed by immediate breast reconstruction. Br J Surg. 2012; 99:799–806.
Article6. Adam H, Bygdeson M, de Boniface J. The oncological safety of nipple-sparing mastectomy: a Swedish matched cohort study. Eur J Surg Oncol. 2014; 40:1209–1215.
Article7. Yang X, Zhu C, Gu Y. The prognosis of breast cancer patients after mastectomy and immediate breast reconstruction: a meta-analysis. PLoS One. 2015; 10:e0125655.
Article8. Reddy S, Colakoglu S, Curtis MS, Yueh JH, Ogunleye A, Tobias AM, et al. Breast cancer recurrence following postmastectomy reconstruction compared to mastectomy with no reconstruction. Ann Plast Surg. 2011; 66:466–471.
Article9. Gerber B, Krause A, Dieterich M, Kundt G, Reimer T. The oncological safety of skin sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction: an extended follow-up study. Ann Surg. 2009; 249:461–468.
Article10. Moon HG, Han W, Noh DY. Comparable survival between pN0 breast cancer patients undergoing sentinel node biopsy and extensive axillary dissection: a report from the Korean Breast Cancer Society. J Clin Oncol. 2010; 28:1692–1699.
Article11. Ota D, Fukuuchi A, Iwahira Y, Kato T, Takeuchi M, Okamoto J, et al. Clinical outcome of reconstruction with tissue expanders for patients with breast cancer and mastectomy. Clin Breast Cancer. 2014; 14:339–345.
Article12. Lee TJ, Hur WJ, Kim EK, Ahn SH. Outcome of management of local recurrence after immediate transverse rectus abdominis myocutaneous flap breast reconstruction. Arch Plast Surg. 2012; 39:376–383.
Article13. Torresan RZ, dos Santos CC, Okamura H, Alvarenga M. Evaluation of residual glandular tissue after skin-sparing mastectomies. Ann Surg Oncol. 2005; 12:1037–1044.
Article14. Barton FE Jr, English JM, Kingsley WB, Fietz M. Glandular excision in total glandular mastectomy and modified radical mastectomy: a comparison. Plast Reconstr Surg. 1991; 88:389–392.
Article15. Doddi S, Singhal T, Kasem A, Desai A. A single institution experience with skin sparing mastectomy and immediate breast reconstruction. Ann R Coll Surg Engl. 2011; 93:382–384.
Article16. Eriksen C, Frisell J, Wickman M, Lidbrink E, Krawiec K, Sandelin K. Immediate reconstruction with implants in women with invasive breast cancer does not affect oncological safety in a matched cohort study. Breast Cancer Res Treat. 2011; 127:439–446.
Article17. Patel RT, Webster DJ, Mansel RE, Hughes LE. Is immediate postmastectomy reconstruction safe in the long-term? Eur J Surg Oncol. 1993; 19:372–375.18. Patterson SG, Teller P, Iyengar R, Carlson GW, Gabram-Mendola SG, Losken A, et al. Locoregional recurrence after mastectomy with immediate transverse rectus abdominis myocutaneous (TRAM) flap reconstruction. Ann Surg Oncol. 2012; 19:2679–2684.
Article19. Newman LA, Kuerer HM, Hunt KK, Kroll SS, Ames FC, Ross MI, et al. Presentation, treatment, and outcome of local recurrence afterskin-sparing mastectomy and immediate breast reconstruction. Ann Surg Oncol. 1998; 5:620–626.
Article20. Pinel-Giroux FM, El Khoury MM, Trop I, Bernier C, David J, Lalonde L. Breast reconstruction: review of surgical methods and spectrum of imaging findings. Radiographics. 2013; 33:435–453.
Article21. Mallon P, Feron JG, Couturaud B, Fitoussi A, Lemasurier P, Guihard T, et al. The role of nipple-sparing mastectomy in breast cancer: a comprehensive review of the literature. Plast Reconstr Surg. 2013; 131:969–984.22. Murthy V, Chamberlain RS. Defining a place for nipple sparing mastectomy in modern breast care: an evidence based review. Breast J. 2013; 19:571–581.
Article23. Spear SL, Hannan CM, Willey SC, Cocilovo C. Nipple-sparing mastectomy. Plast Reconstr Surg. 2009; 123:1665–1673.
Article24. Ponzone R, Maggiorotto F, Carabalona S, Rivolin A, Pisacane A, Kubatzki F, et al. MRI and intraoperative pathology to predict nipple-areola complex (NAC) involvement in patients undergoing NAC-sparing mastectomy. Eur J Cancer. 2015; 51:1882–1889.
Article25. Gouy S, Rouzier R, Missana MC, Atallah D, Youssef O, Barreau-Pouhaer L. Immediate reconstruction after neoadjuvant chemotherapy: effect on adjuvant treatment starting and survival. Ann Surg Oncol. 2005; 12:161–166.
Article26. Prabhu R, Godette K, Carlson G, Losken A, Gabram S, Fasola C, et al. The impact of skin-sparing mastectomy with immediate reconstruction in patients with Stage III breast cancer treated with neoadjuvant chemotherapy and postmastectomy radiation. Int J Radiat Oncol Biol Phys. 2012; 82:e587–e593.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonographic Findings of Postoperative Change after Breast Reconstruction
- Oncologic Outcomes after Immediate Breast Reconstruction Following Total Mastectomy in Patients with Breast Cancer: A Matched Case-Control Study
- Occurrence of contralateral breast cancer in a BRCA-positive breast cancer patient who underwent free TRAM flap reconstruction: a case report
- Breast Lipofilling: A Review of Current Practice
- Expander/Implant Breast Reconstruction after Reconstruction Using an Extended Cutaneous Thoracoabdominal Flap: A Case Report